Keywords
Abstract
Diabetes and its complications derived are among serious global health concerns that critically deteriorate the quality of life of patients and, in some cases, result in lethal outcome. Herein, general information on the pathogenesis, factors aggravating the course of the disease and drugs used for the treatment of two types of diabetes are briefly discussed. The aim of the review is to introduce supramolecular strategies that are currently being developed for the treatment of diabetes mellitus and that present a very effective alternative to chemical synthesis, allowing the fabrication of nanocontainers with switchable characteristics that meet the criteria of green chemistry. Particular attention is paid to organic (amphiphilic and polymeric) formulations, including those of natural origin, due to their biocompatibility, low toxicity, and bioavailability. The advantages and limitations of different nanosystems are discussed, with emphasis on their adaptivity to noninvasive administration routes. The bibliography includes 378 references.
1. Introduction
Diabetes mellitus (DM) is a group of serious chronic diseases associated with endocrine disorder and characterized by high blood glucose levels (hyperglycemia) caused by a combination of genetic, environmental, and behavioral factors, including genetic predisposition, ethnicity, sedentary lifestyle, obesity and others.[1-7] In turn, for the patients suffering from hyperglycemia over prolonged period, macro- and microangiopathy are developed, which can lead to a number of serious and even fatal complications affecting the cardiovascular system, different tissues and organs (nerves, kidneys, foot, eyes, etc.). Among the latter are diabetic neuropathy, diabetic nephropathy, diabetic retinopathy, impaired wound healing, etc.[8-13] According to the International Diabetes Federation (IDF), more than 500 million adults between the ages of 20 and 79 are affected by DM. This number is expected to increase, as the disease is becoming more widespread.[1, 2, 4, 14] According to the IDF data, DM is among the top 10 causes of death worldwide; 4.2 million patients in 2019 and 6.7 million patient in 2021 died of DM.[1, 2, 4, 14] Importantly, in addition to the social and human effects, DM is associated with serious economic burdens. These depressing statistics have led to an increased research attention on the management of DM and its complications.
Generally, two types of diabetes, i.e., type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM), are classified depending on various pathogenesis. T1DM is insulin-dependent diabetes characterized by absolute insulin deficiency due to destruction of pancreatic β-cells. It is typical for young population and mainly caused by genetic predisposition. Patients with T1DM need insulin administration throughout their life. T2DM is characterized by reduced insulin sensitivity with a progressive deficiency in insulin secretion by pancreatic β-cells,[15] thereby resulting in a lack of the hormone in the body. According to statistical data, about 90% of patients with DM have T2DM.[15] Meanwhile, more complex classification may be accepted in some cases, including gestational diabetes.[7] In other cases, authors emphasize the role of insulin deficiency in the etiology and pathogenesis of the Alzheimer’s disease (AD), with insulin resistance in the brain being considered as type 3 diabetes (T3DM).[5]
Diabetes management domain involves a combination of research and clinical strategies focusing on modelling, diagnosis, differentiation, monitoring, drug administration, etc. The diagnosis of DM usually involves the monitoring of glucose levels in body fluids, such as blood (> 125 mg dL–1) and urine. Additional glycemic control may be used by measuring glycated hemoglobin (HbA1c) levels, with an acceptable level of less than 6.5%. Nanomedicine tools for the diagnosis, prediction, prevention and monitoring of DM present a separate line of research, which is mainly remained beyond this review, with only principal points briefly outlined.
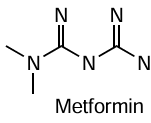
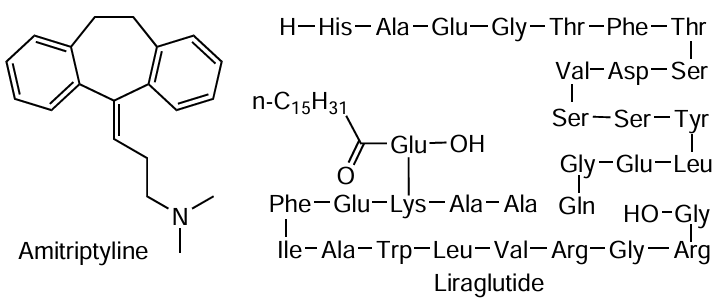
Both types of DM lead to hyperglycemia and require administration of exogenic insulin to keep the metabolic glucose balance. This is conjugated with a number of problems, since (1) conventional treatment of DM occurs through multiple subcutaneous injections of exogenous insulin, which is painful, discomforting and may be the source of infection; (2) there are limited ways of insulin administration, and each has its own weaknesses; (3) unlike low molecular weight drugs insulin is a protein consisting of 51 amino acids (21 and 30 amino acids in chain A and B, respectively) (Fig. 1), which makes it even more difficult to deliver. Despite these challenges numerous efforts are made to develop noninvasive routes of administration, including oral, intranasal, pulmonary, transdermal and others.[3, 16, 17] A variety of antidiabetic drugs are used to treat T2DM, with small molecules showing clear advantages. Classical drugs for these cases are metformin, sulfonylureas, glinides, thiazolidinediones, etc., with metformin being of special importance.[4] Although mechanism of metformin therapeutic effect is not clear, it is suggested that the drug affect liver insulin sensitivity due to controlling glucose production. It is noteworthy that administration of metformin allows both producing hypoglycemic therapy and protection from impaired fasting glucose.
Rapid progress in medicinal chemistry is leading to new generations of drugs with novel mechanisms of action are developed. Much attention is being paid to naturally derived medications[18, 19] due to their affinity to therapeutic targets, safety and availability. First of all, the following antidiabetics should be mentioned: dipeptidyl-peptidase-4 (DPP-4) inhibitors; sodium-glucose cotransporter-2 (SGLT2) inhibitors, glucagon-like peptide-1 (GLP-1) receptors agonists, that belong to a new class of medicines for the treatment of T2DM and its complications, including those with cardioprotective effects.[20] Despite this encouraging information, the occurrence of drug resistance, multitargeted character of the DM, long-term and complicated progression of the disease, existence of additional diseases, and individual sensitivity of diabetic patients to the drug should not be forgotten. These dictate the need to intensify the research activity towards the discovery of new targets and new multitarget therapeutics.[21] Meanwhile, the design of new therapeutic molecules and their bench-to-bedside translation are very expensive and time-consuming processes. Alternatively, essential increase in efficacy of drug therapy can be provided by the use of nanosized carriers, or nanocontainers, that can dramatically modulate the effect of traditional drugs. This is achieved by tuning stability, side effect, targeting properties of drug formulations, as well as their adapting to different administration routes. Since the 1980s, nanotechnology approach finds wide application in medicine, with many generations of drug delivery systems developed for different diseases including oncology, neurodegenerative disorders, inflammatory processes, tuberculosis, DM, etc.[2, 11, 13, 22-24] Typically, these nanocarriers are categorized into several domains, including inorganic, organic (lipid, polymeric) and hybrid.[25, 26] Meanwhile, this is a challenging task to adapt, modify and optimize these nanocontainers to the specific disease, drug and administration route. In view of these facts, effective management of DM and DM-related complications is impracticable outside the nanotechnological approach, which plays an important role in the diagnosis, monitoring, and treatment processes.[2] Application of nanocarriers makes it possible to modify pharmacokinetics and biodistribution of drugs, control their release profile, improve stability, biocompatibility and bioavailability, create depot-like nanoformulations.
Nanomedicine is a dynamically developing field, so to provide the most breakthrough information this review focuses on the most recent publications, primarily covering a period of last one to five years, with the pioneer ideas and approaches highlighted.
Despite the enormous number of publications in the field of diabetes therapy, the structure and content of this review allow it to take its unique place among other recent review publications on this topic. According to the analysis of recent literature, reviews are becoming highly specialized both in terms of medical aspects and in drug formulation development. A significant number of works are devoted to the delivery of a specific drug, primarily insulin, the description of particular administration route, and the use of a certain class of nanocarriers or materials.[3, 6, 9, 17] This review, authored by chemists specializing in drug delivery, includes a classification of systems by both carrier type (lipid, polymer nanocontainers) and delivery route (e.g., oral, transdermal, intranasal, etc.), which allows us to discuss various aspects of modern nanomedicine in the field of diabetes treatment. For a more detailed analysis and understanding of observed trends, forecasting the direction of research and assessing the effectiveness of various systems, it is important to take into account medical aspects, including pathogenesis, etiology of the disease, information on risk factors, stages of disease development, biological targets, involved signalling pathways, etc. Therefore, in addition to chemical, supramolecular and nanotechnological aspects, this review will pay attention to a balanced discussion of biochemical and medical issues necessary to justify the choice of medicinal compositions and nanomaterials.
2. Medicines for the treatment of type 1 and type 2 diabetes mellitus
As described above, DM can be categorized into two main types based on their underlying causes and pathogenesis: type 1 and type 2. The terms used to denote age of onset (juvenile or adult) or treatment type (insulin-dependent or non-insulin-dependent) are considered outdated because these indicators for different types of DM may be similar in some cases.[27] The main reason for the development of T1DM is genetic predisposition,[28, 29] however, viruses (Coxsackievirus) and some poisons (streptozocin (STZ) and rat poison) can have a destructive effect on the pancreatic β-cells. The causes of T2DM are primarily related to metabolic disorders, age, ethnicity, family history, sedentary lifestyle, and unhealthy diet may contribute. Diagnosis of T2DM is complicated by the fact that its symptoms are often mild, and the disease is diagnosed when complications arise several years after its onset.
2.1. Type 1 diabetes mellitus: insulin delivery methods
Insulin, a peptide hormone, is secreted by the β-cells within the islets of Langerhans. Its primary role is facilitating glucose enter into cells of insulin-dependent tissues such as liver, muscles, and adipose.[2, 30] In the pancreas, insulin is predominantly stored as hexamers — structures made up of six insulin molecules that form a stable complex with zinc ions. In this form, insulin remains inactive and cannot interact with cell receptors. Upon release into the bloodstream, these hexamers gradually dissociate into dimers and monomers, which are then able to carry out their biological function. Upon binding to two monomers of the insulin receptor on the cell membrane, insulin triggers their combination into a dimer, initiating the formation of a channel for glucose transport. The stabilization of insulin as hexamers, or conversely, the acceleration of its dissociation into monomers, determines the rate of insulin action. This process is characterized by key parameters such as maximum concentration in the body, time of onset, and action time (Fig. 2). Insulins are categorized into four main types based on their action time: rapid-acting, short-acting, intermediate-acting, and long-acting.[31] Regular human insulin typically needs to be administered 0.5 to 1 hour before meals, which can be inconvenient. To address this, rapid-acting insulins were developed with slight modifications in the amino acid sequence to accelerate the dissociation of dimers into monomers. For instance, Insulin lispro, a human insulin analogue, differs by the reversed sequence of proline and lysine residues at positions 28 and 29 on the B-chain (see Fig. 1).[32] On the contrary, NPH (neutral protamine Hagedorn) insulin includes protamine, which interacts with insulin hexamers, promoting their crystallization and precipitation. This allows to delay the onset of action, but to achieve a more prolonged effect. In addition, to achieve the maximum therapeutic effect, it is possible to use a mixture of different insulins.[33]
Insulin is primarily injected subcutaneously. Recently, there has been a growing focus on noninvasive insulin delivery methods, including the development of systems for oral, intranasal, buccal, pulmonary, transdermal, rectal, vaginal, and ocular delivery.[34-36] Oral insulin delivery remains a promising field of research with significant potential for clinical application,[37, 38] but low bioavailability is a major obstacle to this route of administration. Inhaled insulin Afrezza® [39] is administered through the respiratory tract and is absorbed into the lungs through the pulmonary alveoli. This method is considered convenient and express for patients, but there may be problems in selecting the required dose. Vaginal and rectal insulin delivery involves the use of specialized forms, such as suppositories and gels, which are administered into the vagina or rectum, allowing insulin to be absorbed through the mucous membranes. Despite the advantage of bypassing first-pass hepatic metabolism, the challenges of uncontrolled insulin absorption and potential irritation of the mucous membranes have limited the widespread adoption of these delivery routes.[40] Other noninvasive methods of insulin administration include intranasal and transdermal delivery. These methods could help patients overcome the psychological challenges and risk of infections linked to frequent injections. These routes of insulin administration will be discussed in more detail in this review.
2.1.1. Intranasal insulin delivery
The nasal mucosa is highly vascularized, allowing drugs to be rapidly absorbed into the systemic circulation through transcellular and paracellular transport. The olfactory region in the nasal cavity provides a direct route to the central nervous system, bypassing the blood-brain barrier. For diabetic patients requiring daily insulin, the nasal route offers a viable alternative to subcutaneous injections.[41-43] In addition, the intranasal route of insulin administration is often considered in the context of the neurodegenerative diseases treatment.[44, 45] The intranasal delivery of insulin using various nanocontainers is of utmost interest.
Chitosan and its derivatives are most commonly used in the design of nanocontainers for intranasal delivery. The optimized thermosensitive hydrogel based on 2 wt.% chitosan, 1 wt.% chitosan quaternary ammonium salt, and 0.5 wt.% gelatin showed short gelation time, uniform pore structure, and the ideal swelling rate. These properties facilitated the prolonged release of 65% of encapsulated insulin over 24 hours after intranasal administration.[46] The non-toxic NPs were characterized by a hydrodynamic diameter of 165.3 nm, polydispersity index (PdI) of 0.24, and zeta potential of +21.6 mV.[47] The Krebs – Henseleit buffer was used as a novel diffusion medium in a Franz diffusion cells because of its ability to maintain tissue viability, thereby allowing for more accurate monitoring of insulin penetration efficacy. Chitosan was also commonly used to coat the surface of other nanocontainers. For instance, chitosan-coated insulin-loaded solid lipid nanoparticles (SLN) and poly(lactic-co-glycolic acid) NPs were obtained.[48] Encapsulating insulin in chitosan-coated NP improved structural stability and enhanced nasal absorption. Transfersomes obtained at phospholipids/Tween 80 weight ratios of 10 : 1, 7 : 1, 5 : 1, 3 : 1, and 1 : 1 were modified during hydration of the lipid film with acetate buffer containing chitosan.[49] For example, the shift of the zeta potential from a negative value (–3.5 ± 0.1 mV) to a positive value (+23 ± 4 mV) for the composition with ratio of 3 : 1 indicated the successful coating of the transfersome surface with chitosan. The nasal uptake of insulin encapsulated in transfersomes was validated through fluorescence imaging.
Insulin-loaded fast-dissolving films were developed using the casting method with hydroxypropyl methylcellulose and polyvinyl alcohol.[50] The clinical study of the selected film in post-COVID-19 anosmic patients demonstrated a significant improvement in olfactory detection scores (lower olfactory threshold) in the group of 20 patients.
The insulin-loaded self-emulsifying nanoemulsion (NE) increased insulin permeation three times compared to the insulin solution.[51] In vivo results demonstrated that the Cmax (maximum plasma concentration) and the bioavailability (relative to the subcutaneous delivery) was 255.9 mU mL–1 and 68% (insulin-loaded NE), 5.8 mU mL–1 and 5% (insulin solution). Intranasal delivery of 3.6 IU kg–1 insulin-loaded self-emulsified nanoemulsion significantly reduced plasma glucose level up to 70% with the effect lasting for 4 hours of the experiment.
To prepare arginine-coated self-emulsifying nanoglobule system, lauroyl ethyl arginate was added to a preconcentrate consisting of a medium chain monoglyceride Capmul, a medium chain triglyceride Captex 8000, and a surfactant Kolliphor® RH 40 at a weight ratio of 2 : 3 : 4 (Fig. 3).[52] Insulin loading was achieved by electrostatic binding between the negatively charged α-helix of insulin and positively charged arginine nanoglobules. Following intranasal administration of the insulin-loaded nanoglobule system to diabetic rats at a dose of 2 IU kg–1, a rapid insulin absorption was observed with a significantly higher Cmax = 14.3 mU L–1 and a relative bioavailability of 23.3%. The optimized protamine/insulin formulation after intranasal administration demonstrated blood glucose-lowering activity comparable to subcutaneous insulin.[53] Tissue histology and confocal microscopy revealed that protamine induced rearrangement of adherens junctions in the nasal epithelium, thereby enhancing insulin penetration to the lamina propria for systemic absorption.
Intranasal insulin delivery has been extensively studied and tested due to its ability to achieve the necessary therapeutic levels for DM treatment. This method offers several advantages, including increased bioavailability, painless administration, and usability. Moreover, intranasal insulin delivery is not only beneficial for diabetic patients but has also shown promising results in the treatment of cognitive disorders, such as AD. Drugs administered intranasally can be rapidly absorbed through the nasal mucosa and enter the systemic circulation, which is crucial for quickly achieving therapeutic concentrations in the blood. In addition, intranasal administration allows certain substances to bypass the blood-brain barrier and reach the brain directly. While insulin can be delivered intranasally, this method is not universally applicable for systemic insulin administration. Inhaled insulin, such as Afrezza®, is delivered through the respiratory tract, but not through the nose, to facilitate faster entry into the systemic circulation.[39] Insulin, being a large molecule, has limited absorption through the nasal mucosa into the bloodstream, making intranasal insulin less effective for glucose control compared to traditional methods like subcutaneous injections. At present, noninvasive insulin administration through the nose is still the subject of fundamental research. But it is of great interest in the context of the connection between DM and AD. Intranasal administration may be more suitable for the delivery of small molecules for the treatment of T2DM.
2.1.2. Transdermal insulin delivery
Transdermal delivery offers numerous advantages, including sustained drug release, the maintenance of steady plasma drug level, and enhanced patient compliance.[54] Needle-free injectors, patch, microneedle devices, chemical enhancers, ionophoresis, laser therapy are new techniques to improve the efficiency of insulin delivery through the skin (Fig. 4).[16, 54-56] Moreover, 3D printing technologies are being actively researched to obtain microneedles, also using available raw materials.[57-59]
Innovative patch with heating elements on polyimide substrates for electrothermal transdermal therapy was presented by Pagneux et al.[60] The results demonstrate that adjusting the electrical resistivity of a gold nanohole array patterned on polyimide enables a fast-responding electrothermal skin patch, while a subsequent coating with reduced graphene oxide provides insulin encapsulation capabilities.
Microneedles are needles from 50 to 1000 μm, which can be either soluble or insoluble depending on their purpose and design. Soluble microneedles are made of biocompatible materials (e.g. hyaluronic acid, polyvinylpyrrolidone (PVP), etc.) that dissolve in the skin after injection, releasing active substances. Hollow insoluble microneedles serve as channels for the delivery of drugs. They can be made of metals, silicone, or other solid materials. Drugs are injected through the cavity of the microneedle into the deeper layers of the skin. Zhang et al. proposed polymeric nanocarriers based on carboxymethyl chitosan for insulin delivery, whose penetration through the stratum corneum is facilitated by the use of microneedles.[61] Compared to the transdermal rate of passive diffusion (2.77 ± 0.64 μg cm−2 h−1), the transdermal rate of the insulin-loaded NP is increased by 4.2-fold (10.24 ± 1.06 μg cm−2 h−1) when administered with microneedles.
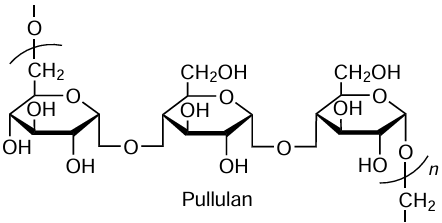
The water-soluble polysaccharide pullulan was used to fabricate microneedles,[62] which dissolved within 2 hours releasing up to 87% of the insulin. After 4 weeks of storage at 4, 20, and 40°C, the insulin successfully retained its secondary structure. Microneedles can be collected on a substrate, such as a patch or roller. A roller with microneedles made of polyvinyl alcohol has been developed for rapid drug delivery across large surface areas.[63] The insulin-loaded roller demonstrated an immediate hypoglycemic effect: lowering blood glucose levels to less than 50% of their original value within one hour of application.
Insoluble microneedles formed by crosslinking gelatin methacrylate with polyethylene glycol diacrylate have been developed.[64] Molybdenum disulfide is added to the microneedles for insulin delivery under near-infrared irradiation. Transdermal administration of insulin using these microneedles significantly lowers blood glucose levels in C57BL/6 mice and mini-pigs achieving effects comparable to subcutaneous insulin injections.
The use of microneedles in combination with ionophoresis significantly enhanced controlled insulin delivery.[65] In this study, the smartphone powered the ionophoresis-driven circuit through its charging port. The natural polymer material (silk fibroin) was often used as a raw material for forming hydrogels for transdermal insulin delivery.[66-68] Poly(3,4-ethylenedioxythiophene):polystyrene sulfonate as a drug carrier and silk fibroin as a hydrogel matrix were used for the transdermal delivery of insulin via ionophoresis allowing precise control of release rate, dosage, and duration.[68] Porous thermoplastic polyurethane was used as a matrix for transdermal insulin delivery.[69] In addition, the ionophoresis technique achieved a twofold increase in insulin penetration through pig skin.
Various types of stimuli-responsive systems are of particular interest. Microneedles that respond to external stimuli have been developed based on metal-organic framework (MOF) made of Co2+ and Zn2+.[70] The MOF in these systems has been used as a storage reservoir for insulin. An increase in glucose levels can trigger the destruction of MOF and the release of insulin. Mesoporous silica NPs with insulin have been incorporated into hyaluronic acid-based dissolving microneedle patch.[71] This smart and elegantly built system consists of the following parts: mesoporous silica NPs as the insulin reservoir, Wulff-type phenylboronic acid (PBA-2) as a sensitive ‘linker’, zinc oxide NPs as gatekeepers. At high blood glucose levels, the stable boronic acid ester formed between ZnO-PBA-2 and diols on the surface of mesoporous silica NPs is completely destroyed, followed by insulin release. In another study,[72] phenylboronic acid (PBA)-modified methacrylate hyaluronic acid was proposed as a base material for microneedle fabrication. In addition, the formation of a covalent bond between PBA and gluconic acid-modified insulin, degrading at high glucose concentrations, was suggested as a stimulus-responsive element. Lin et al. modified multivesicular liposomes with PBA derivatives to confer glucose-sensitive properties.[73] In vitro studies demonstrated the sensitivity of these multivesicular liposomes to pH and H2O2 , attributed to the presence of glucose oxidase (GOx) within the liposomes. Additionally, in vivo experiments showed that when blood glucose levels were reduced to normal, insulin release was decreased.
Microemulsion formulations were successfully obtained using ionic liquids of choline-fatty acids composition as surfactant, Span 20 as a co-surfactant, choline propionate ionic liquid as an internal polar phase, and isopropyl myristate as a continuous oil phase.[74] In vivo transdermal administration of low insulin doses (50 IU kg–1) to diabetic mice revealed that these microemulsion formulations maintained insulin level for a significantly longer period (half-life > 24 hours) compared to subcutaneous injection (half-life = 1.32 hours). In work,[75] optimized insulin-loaded niosome emulgel combination was investigated. The transdermal flux of insulin in the niosome emulgel was ten times higher than that of the insulin solution. In vivo data demonstrated that the insulin niosome emulgel reduced plasma glucose level more effectively than other tested formulations with insulin, including niosome gel, emulgel, gel, and niosomes. Phospholipid derivative 1,2-dimyristoyl-sn-glycero-3-ethyl-phosphatidylcholine as a cation and unsaturated linoleic acid as an anion were used to form ethosomes for transdermal insulin delivery.[76] The formulation with 35% ethanol was identified as the lead candidate. These ethosomes effectively encapsulated insulin with an encapsulation efficiency of 99% and showed long-term stability at both 4°C and 25°C.
Three different deep eutectic solvents were investigated as chemical penetration enhancers for transdermal administration of insulin across rat skin: choline chloride/urea, choline chloride/glycerol, and choline chloride/ethylene glycol, each in a 1 : 2 molar ratio.[77] The cumulative insulin permeation over 24 hours was 131.0, 89.4, and 29.6 mg cm−2 in the presence of choline chloride/ethylene glycol, choline chloride/glycerol, and choline chloride/urea, respectively.
A water-in-oil NE system was developed for percutaneous insulin delivery, consisting of 5 wt.% oleic acid as an oil phase, 60 wt.% Tween 80 as a surfactant, and isopropyl alcohol as a co-surfactant (in a 3 : 1 weight ratio), with 35 wt.% water as an aqueous phase.[78] The optimized formulation was characterized by a small droplet size (41.05 ± 8 nm), a high entrapment efficiency (93.08%), and a notable flux (1.75 μg cm–2 h–1). Сircular dichroism spectra indicated minor conformational changes in the insulin structure due to its entrapment within the NE, indicating that the hormone retained its biological functions.
Advances in transdermal technologies, such as microneedles, ionophoresis, and chemical enhancers, have shown their effectiveness in insulin delivery through the skin. Although further research is needed to optimize these systems and confirm their safety and efficacy, recent trends highlight the potential of transdermal drug delivery for DM treatment. A combination of different methods, for example, NPs with microneedles, microneedles with ionophoresis, to enhance transdermal delivery is particularly promising.
2.2. Type 2 diabetes mellitus: drugs and administration routes
T2DM is much more common than other forms of the disease.[79] Its peculiarity is that the body’s cells become less sensitive to insulin, which means that insulin loses its ability to transport glucose to the tissues. The pancreas perceives this as a signal of insulin deficiency and begins to produce it with increased intensity. As a result, the β-cells of the pancreas, responsible for producing insulin, become depleted over time, and the person is forced to resort to insulin injections.
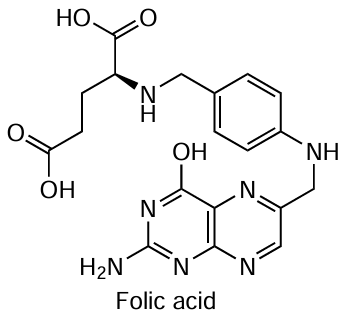
There are several classes of drugs used to treat T2DM, each with its own mechanism of action and route of administration (Fig. 5). Many medications for T2DM treatment are designed for oral administration, which, despite its advantages, has several drawbacks: first-pass metabolism, ‘peak and valley’ pharmacokinetic profile, and low degree of absorption in the gastrointestinal tract.
Metformin (1,1-dimethylbiguanide) is the first-line treatment for T2DM because of its strong glucose-lowering effects, proven safety profile, and affordability. In the form of hydrochloride, it is easily soluble in water. It is administered orally in tablet or liquid form. Metformin treatment is associated with moderate weight loss in patients and, with long-term use, a reduction in cardiovascular risk, as well as antioxidant and anti-inflammatory effects.[80, 81] At this stage, metformin is considered as a polyfunctional drug that can be used to treat various diseases. In addition to the treatment of DM, metformin is also used to treat glucose intolerance, obesity, and polycystic ovary syndrome.[82] Metformin is attracting attention as a potential anticancer agent. In DM management, metformin decreases hepatic glucose production through activation of adenosine monophosphate-activated protein kinase and increases insulin sensitivity in peripheral tissues. Metformin also reduces the rate of glucose absorption in the intestine, which helps to reduce postprandial (after a meal) hyperglycemia. However, metformin is not without negative side effects, including digestive upset, vitamin B12 deficiency, lactic acidosis, and kidney problems. To minimize side effects and unlock the potential of metformin, active fundamental and applied research with this drug is ongoing.
Sulfonylureas (e.g., Glipizide, Glyburide, Gliclazide) and meglitinides (e.g., Repaglinide, Nateglinide) are administered orally in tablet form. Sulfonylureas bind to β-cells of the pancreas and inhibit the adenosine triphosphate-sensitive potassium channels, reducing potassium efflux and causing β-cell membrane depolarization. This depolarization opens calcium channels, allowing calcium influx and increasing intracellular calcium levels, which in turn stimulates insulin secretion from the pancreatic β-cells.[83, 84] Meglitinides (glinides) also bind to β-cells as sulfonylureas, but with less affinity, which reduces the risk of hypoglycemia.
Thiazolidinediones (e.g., Pioglitazone, Rosiglitazone) are also used orally. Through the activation of peroxisome proliferator-activated receptors, thiazolidinediones modify the expression of genes responsible for glucose and lipid metabolism, leading to enhanced blood sugar regulation and reduced triglyceride levels.[85, 86] Thiazolidinediones also increase the sensitivity of tissues to insulin. However, these medications are associated with a wider range of side effects (weight gain, edema, and an increased risk of heart failure) and are expensive.
DPP-4 inhibitors (e.g., Sitagliptin, Linagliptin, Gemigliptin) are a class of medications known as gliptins. They function by elevating levels of incretins, namely GLP-1 and glucose-dependent insulinotropic peptide, thereby enhancing insulin secretion in the blood.[87-89] They are available in tablet form for oral administration. DPP-4 inhibitors are weight neutral and well tolerated.
SGLT2 inhibitors (e.g., Canagliflozin, Dapagliflozin, Empagliflozin) prevent the reabsorption of glucose in the kidneys, which leads to the excretion of glucose in the urine (glycosuria).[90] In addition to their glucose-lowering effects, SGLT2 inhibitors also help to prevent the onset of chronic kidney disease and reduce the incidence of cardiovascular complications in patients with T2DM.[91] This helps to lower blood glucose levels. Medications of this class are used in oral tablet form either as monotherapy or in combination with other antidiabetic drugs.
GLP-1 receptor agonists (e.g., Exenatide, Liraglutide, Semaglutide) enhance the secretion of insulin by b-cells of the pancreas in response to increased blood glucose level and inhibit the secretion of glucagon by a-cells of the pancreas, which reduces the production of glucose by the liver.[92] Route of administration of these large molecules is subcutaneous injection.
Therefore, the primary classes of drugs for treating T2DM include metformin, sulfonylureas, DPP-4 inhibitors, SGLT2 inhibitors, and GLP-1 receptors agonists, each providing unique mechanisms of action and benefits. These medications are typically administered in tablet form, although injectable options are available for some, such as GLP-1 receptors agonists and insulin. Personalized treatment plans that consider the patient’s health profile are crucial for effective management of T2DM, aiming not only to regulate blood glucose levels but also to reduce associated risks such as cardiovascular events and chronic kidney disease.
3. Supramolecular strategies for the construction and modification of nanocontainers for diabetes therapy
The continuous and intensive development of supramolecular chemistry has brought medicine, in particular the field of drug delivery, to a new quality level. The demand for nanoscale delivery systems and the increasing publication activity can be attributed to (1) the simplicity of supramolecular structure assembling, (2) the possibility of fine-tuning of NP properties, and (3) the enhanced bioavailability, improved biocompatibility, and drug targeting facilitated by encapsulation in nanocarriers, which in turn leads to reduced toxicity of pharmaceutical substances.[93, 94] In addition, the use of nanoscale drug delivery systems makes it possible to reduce the drug dosage, control the onset of its action, and regulate the release rate, which is especially relevant in the context of DM therapy.[95] Currently, a multitude of nanocontainers with diverse nature (organic, inorganic, and hybrid) are being developed for the treatment of various diseases, including DM. Supramolecular structures for DM therapy can be constructed through electrostatic interactions,[96] host-guest interactions,[97] hydrophobic effect,[98] and intra- and/or intermolecular π – π stacking interactions.[99] The nanocontainers required for the drug delivery routes used have now been developed. In DM therapy, research has focused primarily on improving the efficacy of drugs for oral administration.[100-102] Nonetheless, there are also studies exploring transdermal [103] and intranasal [104, 105] drug administration (Table 1). The search for alternatives to intravenous administration is driven mainly by the inconvenience and pain associated with it, which leads to poor patient adherence to treatment regimens. At first sight, alternative routes of drug administration offer significant advantages over intravenous route, but they also have disadvantages, which means that researchers need to carefully select drug delivery systems and their components.
Another important challenge in DM therapy is the controlled release and targeted drug delivery. For example, systems responsive to blood glucose levels,[115] stomach pH [116] or both stimuli [117] are known. It is worth noting that a substantial amount of research is focused on the development of an oral form of hypoglycemic drugs, and responsiveness to environmental pH is one of the key factors in the effectiveness of the therapy. pH-Sensitive systems include polymeric nanocontainers, which can undergo protonation and ionization in response to pH changes. This property can be utilized both for protecting the nanocontainer and for the controlled release of drugs. For instance, nanocarriers based on poly((2-dimethylamino)ethyl methacrylate) [109] and the natural biopolymer alginate [110] released only 15 – 20% of drug at acidic pH. In contrast, at pH 7.4, the release of the drugs was significantly higher due to the NP swelling.[118, 119] Similar results were obtained for MOF based on FeCl3 · 6 H2O and 2-aminoteraphtalic acid with zwitterionic polymethacrylate Eudragit® L100-55. Additionally, this system included a mixture of sodium bicarbonate and citric acid as a pH-controlled generator of CO2 bubbles, which accelerated the unpacking of the capsules at neutral pH.[120] Another promising approach is to form NPs with vitamin B12, which at low pH values can form a strong bond with the negatively charged components of NPs and prevent premature drug release.[121, 122] To create glucose-responsive NPs, their surface can be conjugated with phenylboronic acid,[123-125] glucose oxidase [126] or concanavalin A (Con A).[117, 127] GOx and Con A are proteins with lower specificity and stability compared to PBA.[128] As shown in Figure 6, glucose-sensitive fragments can be conjugated to various nanocontainers for the delivery of insulin and other hypoglycemic drugs. GOx is capable of oxidizing β-D-glucose to glucono-1,5-lactone, which spontaneously hydrolyzes to gluconic acid with the formation of hydrogen peroxide (Fig. 6a). In this case, nanocontainers, mainly polymeric, respond to changes in the pH of the environment, swelling and releasing the drug into the blood in response to high glucose levels.[129] The mechanism of action of Con A involves specific binding to glucose through noncovalent interactions, which leads to changes in aggregate morphology and the subsequent release of the drug (Fig. 6b).[130, 131] PBA and its derivatives have attracted considerable attention due to their stability and ease of modification. PBA exists in water in a dynamic equilibrium between a neutral and a negatively charged form (Fig. 6c). The negatively charged form of PBA is capable of binding glucose, whereas the uncharged form can convert to the charged form. This reversible transition between water-soluble and insoluble forms in response to glucose level has led to the development of various glucose-responsive drug delivery systems, including polymer carriers such as hydrogels, microgels, microcapsules, etc. However, due to the high pKa values of PBA (8 – 9), its glucose responsiveness under physiological conditions (pH 7.4) is limited. Consequently, researchers have focused on lowering its pKa values by introducing electron-withdrawing substituents into the benzene ring (such as carboxyl groups, halogens, and nitriles).[128, 132, 133] In addition to conjugating PBA to various types of nanocarriers, another noteworthy strategy involves crosslinking PBA and its derivatives directly to insulin, creating ‘smart insulins’. For instance, Chou et al. synthesized a class of insulin derivatives that contain both an aliphatic segment, designed to bind to serum albumin or other hydrophobic components in the bloodstream to prolong the half-life, and a PBA moiety.[134] These novel insulin conjugates demonstrated a more rapid restoration of normal blood glucose levels in mice compared to standard insulin and clinically used long-acting insulin derivatives in vivo. In another study, PBA, specifically 3-fluorophenylboronic acid, was conjugated with long-acting insulin (insulin glargine, marketed as Lantus®).[135] It was found that attaching the hydrophobic residues of 3-fluorophenylboronic acid to the C-terminus of the A-chain of insulin increased its solubility without compromising its efficacy. Ohno et al. also successfully synthesized a modified PBA-insulin conjugate to evaluate its glucose-lowering activity and cellular adhesion properties.[136] It was demonstrated that subcutaneous injection of the conjugate, in contrast to intravenous injection, exhibited low activity in reducing glucose level. It is worth noting that there is currently significant interest in modifying various nanocarriers with the aforementioned glucose-sensitive compounds. Both in vitro and in vivo studies have shown that NP can not only protect the drug but also regulate the drug release rate according to the glucose concentration in the body. It is important to note that while the primary focus in DM therapy is on lowering glucose level, it is equally crucial for the drug formulation to respond to hypoglycemia. This concept was proposed by Dong et al. and includes the development of a painless and flexible system for regulating blood glucose levels consisting of glucose-loaded pressure-responsive nanovesicles, insulin-loaded black phosphorus nanosheets, as well as hydrogel applied via patch.[137]
Currently, there are various methods for drug delivery, numerous types of nanosystems, and ways to modify them for specific requirements, but how can the appropriate type of NP be selected for the delivery of antidiabetic drugs? Despite the diversity of nanocontainers, there are requirements that all systems must meet, namely biocompatibility and low toxicity. Failure to meet these requirements can often be a limiting factor in the approval of drugs by the Food and Drug Administration (FDA). Nowadays, the majority of NPs among FDA-approved drugs (since 2016) are represented by liposomal (22% or 43% if including lipid-based NP) and polymeric (29%) nanocarriers.[138] This is due to their low toxicity, as well as the relative ease of modifying the NP properties through covalent and noncovalent interactions. Although the number of FDA-approved lipid and polymer nanocarriers for DM therapy is limited, innovative delivery systems for insulin and other hypoglycaemic agents are being researched to improve the efficacy and safety of DM treatment. Research and development in this area is ongoing, and future advances may lead to the approval of new drugs for DM therapy utilizing nanotechnologies.
3.1. Lipid formulations: from classical liposomes to noncovalently modified vesicular nanosystems
The first mention of lipid vesicles dates back to the 1960s, marking an important milestone in the development of new drug formulations with improved properties. The second important step was the FDA approval of Doxil®, the first liposomal anticancer drug doxorubicin, for clinical use. Due to low toxicity, improved biocompatibility, ability to encapsulate hydrophobic and/or hydrophilic substrates, etc., lipid-based drug delivery systems are increasingly reaching clinical applications (more than 20 to date) compared to other types of nanocontainers.[139] In the context of DM therapy, the main challenges are (1) protection of hypoglycemic drugs from premature chemical and enzymatic degradation, (2) overcoming biological barriers, (3) controlled drug release (stimulus-responsive systems), (4) high encapsulation efficiency.[140]
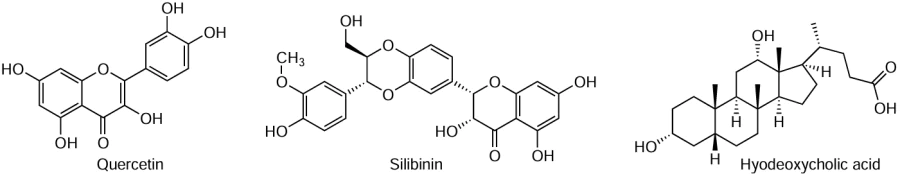
The DM pathogenesis can be slowed down by using natural ingredients obtained from medicinal plants. An example of such compounds is quercetin, which has antioxidant and anti-inflammatory activities. Incorporation of quercetin into soy phosphatidylcholine and cholesterol liposomes has been shown to reduce oxidative stress, inflammation, endoplasmic reticulum stress, and autophagy in pancreatic tissue in a rat model of T1DM.[141] It is worth noting that the efficacy of quercetin encapsulated in conventional liposomes, i.e., phospholipids (or a mixture of lipids), cholesterol and sometimes polyethylene glycol (PEG), has been repeatedly demonstrated, making this therapeutic strategy promising for addressing both insulin resistance and the associated inflammation.[142] Another example of a natural therapeutic agent with similar properties is silibinin (or silybin), which has been shown to normalize blood glucose levels, enhance insulin sensitivity in cells, and improve pancreatic β-cell function, as confirmed by in vivo experiments.[98, 143] It is worth noting that the classical liposome composition is safe and non-toxic for both oral and transdermal delivery of antidiabetic drugs.[144]
Liposomes are very ‘flexible’ type of nanocarrier, since they can be used in their classical composition, modified with various ligands to confer specificity of action, and loaded with both hydrophilic and hydrophobic substrates. Additionally, their size, charge, and the number of bilayers can be varied. This versatility explains their continued popularity as one of the most sought-after delivery systems.[145] While monolayer liposomes of classical composition have been described above, Tian et al. developed multilamellar liposomes for intramuscular injection of exendin-4. Exendin-4 has a short half-life in the body, which is around 2.4 h, however, encapsulating it in liposomes modified with palmitic acid (with encapsulation efficiency of > 99%) extended its half-life to 77.28 ± 12.92 hours.[146]
One of the main properties of liposomes is to increase the bioavailability of drugs. At the same time, through various modifications of the vesicle composition, their therapeutic effect can also be enhanced. Such modifying agents include hyodeoxycholic acid, which can induce insulin secretion. It has been shown that the content of hyodeoxycholic acid directly affects the physicochemical characteristics of the vesicles. Increasing the concentration of hyodeoxycholic acid increases the hydrodynamic diameter of the liposomes from 196 nm to 332 nm and decreases the encapsulation efficiency of metformin from 67% to 59%. Furthermore, in vivo experiments have established that the most optimal system is liposomes with a 1 : 1 mass ratio of hyodeoxycholic acid to metformin (compared to ratios of 0.5 : 1 and 2 : 1). Oral administration of this composition significantly reduces glucose levels, bringing it close to the level of healthy animals and even slightly lower than in the group receiving free metformin.[147]
As noted earlier, liposomes as drug delivery systems occupy a leading position both in the market of nanosized dosage forms and in the field of scientific research. Most liposomal drugs currently available on the market have a classical composition.[22] However, despite their advantages, conventional liposomes have several limitations, such as low stability, rapid elimination from the body, non-targeted drug delivery, etc. As a result, the current trend in the literature is increasingly focused on the development of nanocontainers with improved properties through the incorporation of specific ligands. The primary goals of these modifications are to increase the circulation time of liposomes in the body, achieve controlled drug release, enhance targeting, improve the stability of liposomes during storage, and adapt them to various routes of administration.[148] This research has led to the development of next-generation lipid nanocontainers that have been successfully tested for the DM treatment.
3.1.1. Application of surfactants for creation and modification of nanocontainers
In addition to the degradation of nanocarriers in the gastrointestinal tract, low oral bioavailability of drugs may be due to first-pass metabolism, limited drug solubility and permeability.[149, 150] As a result, conventional NPs are not always suitable (or insufficiently effective) for oral drug delivery, which motivates researchers to develop new, adapted systems. Surfactants are a vast class of compounds and serve as versatile tools for creating a wide range of NPs with enhanced properties due to their amphiphilic nature and structural diversity. Among the most well-known nanocontainers obtained using surfactants are transfersomes and transethosomes,[151-153] cationic liposomes,[154-156] micro- and nanoemulsions,[157-159] niosomes,[160-162] bilosomes,[163, 164] etc. (Fig. 7).
3.1.1.1. Bilosomes
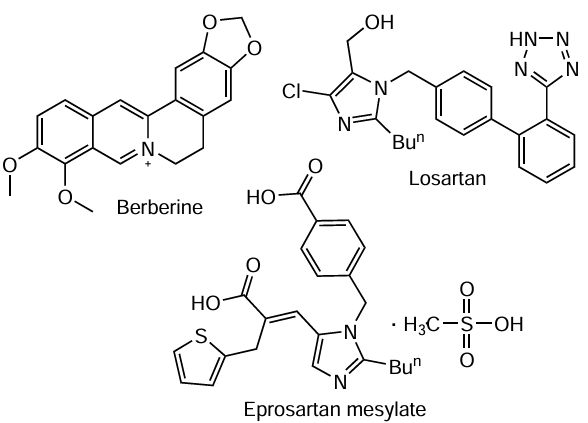
In the context of oral drug delivery, a relatively new type of nanocontainers — bilosomes — is of particular interest. The main components of bilosomes are nonionic surfactants (Span, Tween), bile salts (more commonly sodium deoxycholate), and lipids. Bile salts also act as biosurfactants, repelling external bile salts present in the intestinal lumen, thereby protecting the aggregates and the drug from degradation.[165] Since their first mention by Conacher et al. in 2001,[166] bilosomes have been tested for the therapy of various diseases, including oncological and neurodegenerative. They have also been adapted for transdermal and ocular drug delivery.[167] In DM management, Soliman et al. developed lactoferrin-coated bilosomes for oral delivery of the flavonoid quercetin.[168] Based on the results of in vitro, ex vivo, and in vivo experiments, the authors demonstrated a significant enhancement of the antidiabetic effect of bilosomes due to the synergistic effect of lactoferrin and quercetin, specifically owing to their hypoglycemic, anti-inflammatory, and antioxidant properties. In another study, the effectiveness of bilosomes in enhancing the oral bioavailability of berberine (an isoquinoline alkaloid) was evaluated for the first time. The authors found that bilosomes exhibited optimal characteristics with a concentration of phosphatidylcholine at 0.06 mol L–1, 25 mg of sodium deoxycholate, and 15.2 mg of cholesterol. It is important to note that the size of bilosomes and their encapsulation efficiency are primarily influenced by the cholesterol content, while the zeta potential is affected by the concentration of nonionic surfactants and bile salts.[169, 170] Pharmacokinetic experiments revealed a 6.4-fold increase in the relative bioavailability of berberine when loaded into nanocontainers compared to the free form of the alkaloid. Although the authors found a 99.3% and 31.7% pharmacological effect in reducing blood glucose levels for the formulated and free berberine, respectively, subcutaneous insulin injection remains more effective.[170] It is worth noting that the literature includes studies on loading bilosomes with first-line DM medications, i.e., insulin for oral delivery and metformin hydrochloride for transdermal delivery.[113, 171] However, bilosomes can be used not only for lowering blood glucose levels but also for addressing the complications and consequences of DM, such as diabetic nephropathy. In vivo studies have demonstrated the nephroprotective effects of eprosartan mesylate and losartan-loaded bilosomes upon oral administration.[172, 173]
3.1.1.2. Niosomes
Another example of an effective dosage form containing surfactants is niosomes. Due to their composition (nonionic surfactants and cholesterol), niosomes exhibit lower toxicity compared to other types of NP and can be administered via various routes, including oral, transdermal, ophthalmic, and pulmonary.[174] According to years of research in the field of drug delivery systems, niosomes are promising vehicles for dermal and transdermal drug delivery.[175] For instance, the classic drug metformin hydrochloride was encapsulated in niosomes for transdermal administration to extend its antidiabetic effect and to explore its ability to enhance wound healing in diabetic patients.[176] The authors of the study claim that transdermal administration of metformin hydrochloride every 2 days provides a more sustained antidiabetic effect compared to daily oral administration of metformin. Additionally, the niosomal formulation demonstrated wound-healing activity by improving wound contraction and collagen deposition, and by stimulating serum transforming growth factor beta (TGF-β) level, which is also a significant outcome in the context of DM therapy.
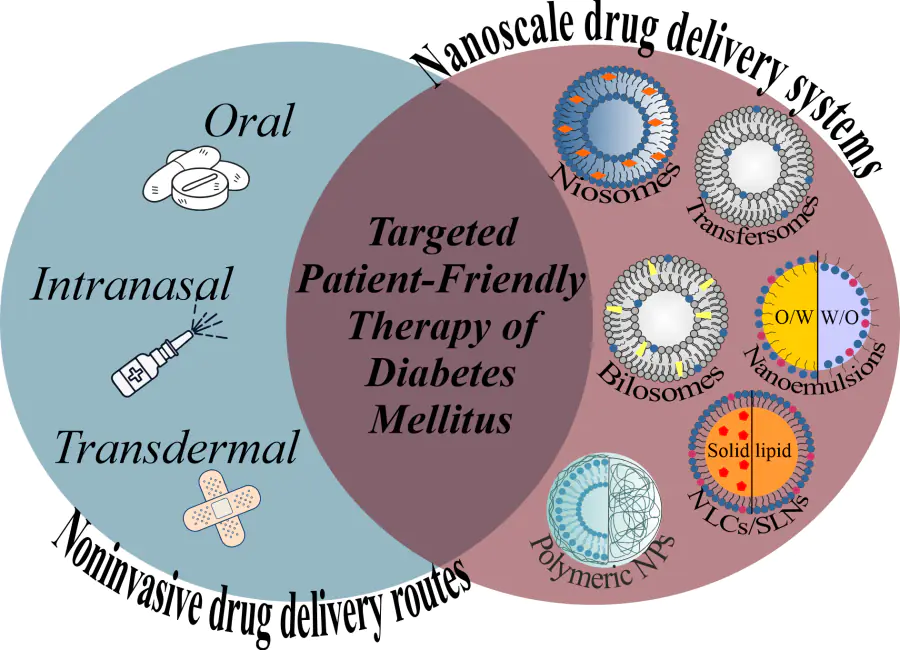
One of the advantages of niosomes (as well as other lipid-based nanocontainers) is their ability to encapsulate drugs over a wide range of solubility. Due to their bilayer structure, niosomes can encapsulate both hydrophobic (within the bilayer) and hydrophilic compounds (within the aqueous core). Dual loading of substrates into nanocontainers has been and remains a highly attractive strategy, as it not only enhances therapeutic efficacy but also targets multiple sites and produces a synergistic effect. This approach has also been applied in DM therapy for one of the most widely used drugs – hydrophobic glipizide and hydrophilic metformin.[177] The main idea of this work is to develop a drug formulation based on a suspension, which could make oral administration of antidiabetic medications more convenient, especially for patients with dysphagia. Pursuing the same goal, the authors of the [178] developed chewable tablets containing niosomes with repaglinide. It was found that encapsulating metformin and glipizide in niosomes results in a more prolonged release of the drugs, which potentially addresses the issue of their short half-life (less than 6 hours) and, consequently, reduces the frequency of medication administration. In another study, Eissa et al. formulated proniosomal compositions loaded with amitriptyline and liraglutide for the treatment of diabetic peripheral neuropathy.[179] In this study, the strategy was different: amitriptyline, used for treating diabetic neuropathy, can lead to hyperglycemia, which is a major drawback. Combination therapy with amitriptyline and an antihyperglycemic agent (liraglutide) can provide effective treatment for neuropathic pain while also managing blood glucose level. Moreover, the developed formulation enables the replacement of the currently available injectable form of liraglutide with an oral one. Interestingly, not only drugs can be combined, but also drug delivery systems. For example, novel deformable liponiosomal hybrids have been developed, combining components of both liposomes and niosomes (phospholipids, cholesterol, nonionic amphiphiles Span 60 and Tween 80), for oral delivery of repaglinide.[180] Researchers are also highly interested in the antidiabetic properties of plant-based medicinal compounds encapsulated in niosomes.[181-183]
3.1.1.3. Transfersomes and transethosomes
Another well-known example of modifying the properties of lipid nanocontainers with amphiphilic molecules is the creation of ultra-deformable liposomes – transfersomes – by incorporating edge activators, most of which are nonionic surfactants, into the lipid bilayer. Transfersomes were first proposed in 1992 as transdermal drug delivery systems by Cevc et al.[184] Eleven years later, in 2003, Cevc published a review on the potential of ultra-deformable carriers for transdermal insulin delivery.[185] It is noteworthy that there are references to clinical studies conducted with transfersomes loaded with insulin and ketoprofen.[186, 187] Over the years, transfersomes have been tested for transdermal delivery of classic hypoglycemic drugs such as insulin[188] and metformin hydrochloride,[111] as well as pioglitazone and eprosartan mesylate for combined therapy against hypertension and DM.[189] For all compositions tested in the STZ-induced model of DM, an improved glucose-lowering effect was observed in rats compared to the free and/or oral forms of the drugs. It is worth noting that transfersomes have ‘siblings’ – transethosomes – which have also been successfully used for loading antidiabetic drugs.[190, 191] The only difference between transethosomes and transfersomes is that transethosomes contain ethanol to enhance the penetration of aggregates through the skin. Transfersomes and transethosomes have also been successfully used as delivery systems to address complications caused by DM, particularly for promoting the diabetic wound healing.[192, 193]
Thus, the strategy of modifying liposomes with surfactants is quite promising. Special attention should be paid to other lipid nanocarriers containing surfactants, such as SLN, nanostructured lipid carriers (NLC), and NE, as they offer certain advantages over liposomes, including improved stability, controlled drug release, higher drug loading capacity, and easier production and scalability.
3.1.2. SLN, NLC, NE
Despite the advancements achieved by researchers in the development of liposomal delivery systems for antidiabetic drugs, several significant challenges remain, such as premature drug leakage, limited stability, low targeting ability, nonspecific clearance, and difficulties in scaling up production.[194] To address these issues, the next generation of lipid nanocarriers has been developed, specifically solid lipid nanoparticles and nanostructured lipid carriers. The primary components of SLN are biodegradable and biocompatible solid lipids (e.g., 1-tetradecanol, cetyl palmitate, various triglycerides, etc.) and surfactants (such as sodium lauryl sulfate, Tween, Precirol® ATO-5, etc.). In contrast, NLC include these components along with liquid lipids or oils (castor oil, Labrafac™ CC, oleic acid, etc.).[195] Another example of such systems is NE, which are fine water-in-oil (w/o) and oil-in-water (o/w) dispersions of two immiscible fluids. Nanoemulsions — emulsions with droplet sizes ranging from 20 to 100 nm — are kinetically stabilized dispersions formed by combining and stabilizing two immiscible phases using a surfactant. Due to their small droplet size, they possess characteristics such as high surface area per unit volume, high stability, optically transparent appearance, and improved bioavailability of drugs.[196, 197] The primary components of these systems include various semisynthetic oily esters, triglycerides, partial glycerides, and nonionic ester emulsifiers. It is important to note that emulsifiers with high hydrophile-lipophile balance (HLB) values (8 – 18) are used to produce o/w NEs, while emulsifiers with low HLB values (3 – 6) are more suitable for producing w/o NE.[198] Numerous studies have confirmed that SLN, NLC, and NE have low toxicity, high stability and have been extensively studied for the treatment of a wide range of diseases, including DM.
3.1.2.1. Solid lipid nanoparticles
Like any drug delivery system, the composition and physicochemical characteristics of NPs must be thoroughly optimized before testing on animal models. This stage is crucial and requires the preliminary statistical and mathematical data processing. Priyanka et al. optimized the composition of SLN using a central composite design with Design Expert software by varying four factors during NP preparation: homogenization speed and time, as well as sonication time and intensity.[199] The results were monitored by changes in particle size, PdI, and zeta potential of the NPs. The same design method was applied for the development of curcumin-loaded SLN.[200] The authors found that increasing the homogenization speed (up to 15 000 rpm) and time (up to 30 min) reduced particle size and PdI while increasing the zeta potential. Increasing sonication time up to 5 min demonstrated similar results, whereas sonication intensity had minimal impact on the SLN physicochemical characteristics. In another study, the Box-Behnken Design (using Design Expert software) was employed to examine the effects of the drug-to-lipid ratio, surfactant and co-surfactant concentration on SLN size, entrapment efficiency, and PdI.[201] Statistical analysis revealed that the most optimal values for particle size (147.1 nm), entrapment efficiency (83.6 ± 0.8%), and PdI (0.265), which were close to the predicted values, were obtained with a drug-to-lipid molar ratio of 1 : 4.16, 1.21% surfactant, and 0.4775% co-surfactant (Fig. 8). Subsequently, the optimized formulations were loaded with extracts of Ficus religiosa L.[199] and tetrahydrocurcumin,[201] both of which possess antioxidant properties. In vivo, these formulations demonstrated an enhanced ability to lower blood glucose levels compared to the free drugs. In general, compounds with antioxidant properties that are encapsulated in SLN are highly effective for DM therapy and exhibit significant potential.
SLN have been successfully tested for the delivery of glibenclamide,[202] tetrahydrobiopterin,[203] repaglinide,[204] myricetin,[205] and many other therapeutic compounds. Evidently, SLN possess excellent properties, and in addition, like conventional liposomes, they can be modified with various ligands. For example, SLNs loaded with the hydrophilic drug saxagliptin were further coated with the methacrylic acid copolymer Eudragit RS100 to enhance the oral bioavailability of the drug.[206] A similar approach was applied for the transdermal delivery of glibenclamide using NLC coated with Eudragit L.[207] Polymethacrylates can be used to enhance drug penetration through the skin, intestinal epithelium, and cornea, improve bioavailability, serve as enterosoluble coatings, prolong drug release, enable pH-dependent release, etc.[208] In another study, SLNs were adapted for endosomal escape.[209] The authors prepared nanocarriers with pH-sensitive HA2 fusion peptides from influenza virus hemagglutinin, which can respond to the acidic environment in endosomes and initiate escape. It was found that loading HA2 peptides into the outer shell of SLN results in more efficient release of nanocarriers from early endosomes compared to peptides loaded into the aqueous core, leading to increased biological activity of insulin.
3.1.2.2. Nanostructured lipid carriers
NLCs are also being successfully developed for the delivery of hypoglycemic drugs for both oral [210] and transdermal [211] administration. As noted earlier, structurally, NLCs are very similar to their predecessors, but they differ in the inclusion of liquid lipids, resulting in greater stability of NPs. In DM treatment, NLCs have found widespread use both as carriers of hypoglycemic drugs and for healing ulcers and wounds associated with DM. For successful vesicle production, it is crucial to select the right components. The authors of the [212] tested a range of solid lipids at various concentrations (Imwitor® 900 K, Dynasan® 116, Kollivax® GMS II, cetostearyl alcohol), as well as several surfactants (Tween 80, Poloxamer 188, Lecithin, and TPGS) to obtain stable NLCs and load sucupira oil. Using a 22 factorial design, it was established that an optimal sucupira oil-loaded NLCs should consist of 0.5 wt.-vol.% sucupira essential oil, 4.5 wt.-vol.% Kollivax® GMS II, and 1.425 wt.-vol.% TPGS, resulting in a mean particle size ranging from 100 to 200 nm and PdI < 0.3. Overall, plant-based medicines are gaining increasing interest due to their lower toxicity compared to synthetic drugs. For example, silymarin inhibits gluconeogenesis, reduces glucose-6-phosphatase activity, and suppresses the overexpression of the cytochrome CYP 3A2 enzymatic system, contributing to its antidiabetic properties. However, its low water solubility has prompted researchers to create NLCs and investigate the impact of various solid lipids (stearic acid (C18) and cetyl palmitate (C32)) on their efficiency.[213] It was found that both NLC systems reduced glucose and triglyceride levels better than free silymarin in vivo, but the effect of NLCs with stearic acid was more pronounced and lasted longer. The authors argue that as the fatty acid chain length increases, the degradation rate decreases. Additionally, both formulations demonstrated a significant antihyperalgesic effect in diabetic neuropathy in mice. NLCs have also been adapted for the oral delivery of hypoglycemic drugs such as pioglitazone,[214] piperine [215] and glargine insulin,[216] as well as transdermal delivery of repaglinide.[211]
It is necessary to highlight the studies, in which NLCs were used as carriers for the healing of wounds and ulcers caused by DM. Diabetic wound healing is known to be a complex process that involves multiple stages. However, in many cases, severe inflammation leads to improper and consequently prolonged wound healing. For this purpose, the authors of the [217, 218] developed NLC-based systems with various auxiliary components to deliver anti-inflammatory agents 20(S)-protopanaxadiol and pioglitazone. For 20(S)-protopanaxadiol, the authors designed a three-dimensional mesh structure of silicone elastomer loaded with drug-bearing NLCs. In in vivo experiments, it was shown that due to the synergistic action of the wound-healing elastomer and the anti-inflammatory 20(S)-protopanaxadiol, the authors managed to achieve suppression of inflammatory infiltration, stimulation of angiogenesis, and regulation of collagen level during the inflammatory, proliferative, and remodelling phases of diabetic wound healing, respectively.[218] Pioglitazone was loaded into NLCs within a framework of collagen (a structural stabilizer) and chitosan (a controlled drug delivery system). The authors demonstrated a similar synergistic effect in diabetic wound healing in vivo: pioglitazone suppressed the inflammatory phase, while collagen and chitosan promoted cell proliferation and migration, leading to 99% wound healing within 21 days.[217]
3.1.2.3. Nanoemulsions
Over the past decade, there has been a significant increase in the use of NE, especially in the pharmaceutical and cosmetic industries, and DM therapy is no exception. The well-known antioxidant quercetin was loaded into NE for DM therapy. Mahadev et al. investigated the NE form of quercetin and evaluated its combinatory effect with the β-carotene.[219, 220] The process of obtaining NE in both cases was optimized using the Box-Behnken design. It was demonstrated that NE-formulated quercetin, both alone and in combination with β-carotene, exhibited excellent oral bioavailability and significant protective and therapeutic activity against STZ-induced DM over 21 days. This composition allowed control of body weight and blood glucose levels while suppressing high serum lipid levels. To enhance the antidiabetic potential, quercetin was loaded into self-nanoemulsifying drug delivery systems (SNEDDS) along with curcumin, Ganoderma lucidum powder extract, and probiotics. An in vivo pharmacodynamic study demonstrated improved recovery of blood glucose levels, body weight and lipid profile in rats over 42 days of treatment.[221] It is worth noting that quercetin loaded into NE has been investigated in vivo as a cardioprotective agent to mitigate cardiac toxicity and deoxyribonucleic acid (DNA) damage induced by DM.[222] In DM therapy, SNEDDS have been successfully developed for the oral delivery of exenatide-4 [223] and mahogany seed extract (Swietenia mahagoni).[224] Since exenatide-4 has low oral bioavailability due to enzymatic degradation in the gastrointestinal tract, the authors combined it with the chymotrypsin inhibitor chymostatin. It was shown that the pharmacodynamic response after oral administration of the NE was comparable to that of the commercially available oral form of exenatide-4, Byetta®. In another study, SNEDDS based on black seed oil (which contains thymoquinone), Capmul MCM, and Cremophor EL were loaded with sitagliptin and dapagliflozin, encapsulated in hard and/or soft gelatin capsules for the effective treatment of T2DM (Fig. 9).[225] In turn, NE have been used for the delivery of both synthetic drugs (pioglitazone hydrochloride,[226] as well as metformin and repaglinide individually or in combination [227]) and plant-derived substances (glycyrrhizin,[228] 2,4,6-triphenylaniline,[229] berberine,[230] essential oil from Alpinia zerumbet Fructus [231]), whose efficacy has also been demonstrated in vivo. Much of the current research is focused on creating gel forms of NE for better retention on the skin and diabetic wound healing. The pharmaceutical substances chosen for these formulations typically include drugs with antidiabetic, anti-inflammatory, antimicrobial, and wound-healing properties.[232-235] As a gel matrix, substances such as chitosan, hyaluronic acid, alginate, agarose, gelatin, cyclodextrin, carrageenan, fibrin, collagen, dextran, etc. can be used.[236-238]
Thus, the use of lipid nanocarriers encompasses a wide range of applications, from delivering various types of drugs for DM therapy to addressing disease complications. Researchers have learned techniques for controlled drug release, achieving high loading efficiency, and prolonging drug action by modifying nanocarriers with specific ligands, leading to the development of new generations of lipid vesicles. Today, there is a growing global trend to develop new drug delivery systems for DM treatment, to adapt existing systems, and to incorporate drugs of natural origin. This surge in interest is driven by the ease of manipulation and low toxicity of lipid nanocarriers. Polymer nanocarriers, which will be discussed in the following section, also meet these criteria.
3.2. Application of polymers for creation and modification of nanocontainers
In general, oral administration of antidiabetic drugs is preferred, as the dosing and frequency of medication make invasive methods challenging. The gastrointestinal tract, however, presents a wide pH range, a multi-layered mucosal structure, and enzymes reducing the bioavailability of peptides and proteins. Polymer NPs made of various natural biodegradable polymers, as well as synthetic ones are pH-sensitive (Fig. 10). This, combined with their modifiability, high biodegradability, biocompatibility, and stability, provides a broad platform for selecting the appropriate composition for antidiabetic drug delivery. Nanocarriers can either be composed entirely of polymers (polymeric micelles, vesicles, and dendrimers) or polymers can act as modifiers for other NPs, like liposomes, silicone nanospheres, etc.[239]
Polymers occupy a leading position in the field of biomedicine in terms of applicability and scientific research.[240] Review articles emphasize the advantages of polymeric nanocontainers, including precise size control (ranging from 1 to 1000 nm), diverse morphologies (rods, worms, disks, etc.), the capacity to load a wide variety of substances (hydrophobic, hydrophilic, large and small biomolecules), stimulus responsiveness (to pH, redox environment, enzymatic environment, and temperature), as well as their stability, modifiability, etc.[241, 242] Due to these numerous advantages, polymeric nanocontainers are extensively studied for the treatment of some of the most pressing diseases, including cancer,[243, 244] neurodegenerative,[245] cardiovascular,[246] DM and its complications,[247, 248] rheumatoid arthritis [249] and many others. As described above, the majority of FDA-approved NPs are represented by lipid and polymeric nanocarriers.[138] The choice between polymer and lipid nanocontainers depends on the specific goals and conditions of treatment. Polymer nanocontainers may be preferable for sustained, controlled drug release and where high stability is required. Lipid nanocontainers, on the other hand, may be better in cases where high biocompatibility and ease of production are required. With each passing year, more and more research is being conducted in the field of polymer-based drug delivery systems to address the existing limitations. For instance, a common method of increasing the stability of drug carriers is to use polyacids and polybases, which are resistant to pH changes but capable of swelling and degrading. Another example of a responsive system is a nanocarrier with dual sensitivity to both glucose level and pH value. The creation of multifunctional systems that are immediately responsive to several stimuli was pursued in the work of Lin.[73] The authors investigated polymeric vesicles based on glucose-sensitive polyphenylboronic acid and pillar[5]arene, containing GOx for transcutaneous delivery of insulin. The selected formulation demonstrated a rapid response to hyperglycemia and the ability to restore blood glucose concentration to normal level.
For more effective therapy, additional requirements for polymeric NPs, such as the ability to be adsorbed onto mucosal surfaces or to avoid exposure to the immune system, must be taken into account. These factors are particularly important given that transdermal and oral routes are the primary methods for delivering hypoglycemic drugs. These aspects, which will be discussed in following sections, have the potential to significantly enhance the therapeutic efficacy of nanocarriers in DM treatment.
3.2.1. New generation stealth nanoparticles
The use of polymers in drug carrier formulations not only ensures controlled release of the substance but also helps to prevent its clearance. When any nanocarrier enters the human body, a protein corona is formed around it, which can lead to opsonization, phagocytic clearance, the formation of immune complexes, and the activation or suppression of the immune system.[250, 251] One strategy to avoid recognition by the immune system and removal of particles from the body involves coating them with hydrophilic polymers such as PEG, poly(2-oxazoline) (POx), PVP, polyglucoronic acids, etc. (stealth delivery systems).[252, 253] The polymers create a steric hindrance to the interaction of NPs with the surrounding opsonin proteins, making them invisible to phagocytes. The term stealth effect emerged from studies on PEGylated liposomes, which demonstrated prolonged blood circulation compared to conventional non-PEGylated liposomes.[254, 255] Non-PEGylated liposomes exhibit a biphasic clearance, whereas PEGylated liposomes typically exhibit a monophasic clearance with a longer half-life. Stealth effect refers to the ability of nanomaterials to remain invisible to the immune system, particularly to the reticuloendothelial system. Hydrophobic and charged particles tend to be more easily opsonized in the bloodstream.[256, 257] Therefore, to increase their half-life, hydrophilic polymers with flexible structures that can sterically prevent the formation of a protein corona are used, such as the aforementioned PEG and POx,[258] as well as poly(zwitter ions), for example, polysulfobetaine or polycarboxybetaine.[259-261] Additionally, the edges of the polymer coating are sometimes functionalized with cell membrane components or with integrin-associated protein Cd47 (Fig. 11).[253]
PEG is the primary material used for NP surface modification. It coats nanocarriers with a hydrophilic masking surface, providing reduced immunogenicity and phagocytosis, decreased intermolecular aggregation, and increased water solubility and stability in blood. Therefore, these properties promote long-term circulation of NPs in the bloodstream. Various approaches have been used in developing antidiabetic drug delivery systems using PEG. The main methods include encapsulating drugs in polymer NPs made of PEG, covalent binding PEG to drug molecules, and using PEG to modify the NP surface.[262, 263] Numerous studies have repeatedly demonstrated the increased effectiveness of drug delivery systems coated with PEG.[264, 265] One such study was conducted by Reboredo et al.,[266] where NPs based on natural polymer zein, which enhances glucose tolerance by stimulating GLP-1 secretion, were compared with PEG-modified particles. Experiments on mice showed a significant reduction in hyperglycemia and a higher ability to induce GLP-1 secretion in the group of animals treated with NP-PEG compared to those treated with free zein or unmodified NPs. The authors attribute these differences to the fact that unmodified NPs remain in the protective mucus layer, whereas NP-PEG can diffuse through mucus and reach the surface of the intestinal epithelium.
Despite the widespread use of PEGylated systems, some studies have shown that such NPs can induce immune responses, including hypersensitivity, accelerated blood clearance, and antibody production under certain conditions.[267] This makes the use of other polymers or modified PEG a promising direction in the development of new drug carriers.[268] However, attempts to use other polymers, such as POx, as stealth polymers have shown that particles with these polymer coatings can accelerate C1q-mediated complement activation and C3 opsonization (third complement protein) by human phagocytes,[269] despite positive results when administered to mice.[258] Another example of attempts to replace PEG is the work of Ryujin et al.,[270] where researchers demonstrated that modification of liposomes with zwitterionic polycarboxybetaine induced specific immunoglobulin M after the first administration of the optimal dose, and modified liposomes were rapidly cleared from the blood after the second dose due to accumulation in the liver, as previously observed for PEGylated liposomes. Currently, PEG is the most extensively studied polymer for use in pharmaceuticals, with several PEGylated drugs in clinical trials for the treatment of DM (Besremi™, Fulphila™, Neulasta®, Krystexxa®), making PEG modification the most advanced strategy in drug formulation development.[271, 272]
The structure of PEG allows it to be modified with ligands to facilitate NP transport across biological barriers. In some cases, conjugating PEG with biomolecules (such as peptides and antibodies) has been shown to reduce immune responses. One of the therapeutic agents used in DM treatment is GLP-1 receptors agonists (such as semaglutide, exenatide, and oxyntomodulin). However, these agents typically have short half-lives and face challenges in penetrating the intestinal barrier.[273, 274] Thi Nguyen et al. developed monoPEGylated exenatide to extend its half-life in vivo.[275] Monitoring of hypoglycemic activity demonstrated that such modification improve glucose tolerance compared to free exenatide, with the nanocarriers maintaining hypoglycemia 12 – 14 times longer than native exenatide. In addition to peptides and antibodies, folic acid (FA) and glucose can also act as molecules that enhance the penetration of PEGylated particles.[276, 277] FA is one of the gastrointestinal tract receptors capable of enhancing the absorption and transport of biologically active substances. In a study by He et al.,[277] FA conjugated with 1,2-distearoyl-sn-glycero-3-phosphoethanolamine and PEG was used to modify the surface of reversible micelle-lipid nanocapsules (FA-RM-ELNC) to ensure targeted delivery of exenatide and prolong the circulation time of particles. In vitro experiments showed that oral administration of FA-RM-ELNC showed a good hypoglycemic effect in mice with T2DM. Notably, FA-RM-ELNC was able to maintain blood glucose level at 65 to 90%, whereas blood glucose after subcutaneous injection of exenatide solution remained at 80 – 95%, and in the case of RM-ELNC at 80 – 90%.
Addressing the limitations of PEGylated drug delivery systems, Ozer et al. developed poly[oligo(ethylene glycol)methyl ether methacrylate] (POEGMA) as a next-generation polymer, analogous to PEG, for drug conjugation.[278] In the hyperbranched polymer POEGMA, long ethylene glycol sequences are replaced by shorter oligomeric ethylene glycol side chains along the hydrophobic backbone. The approach involves conjugating exendin with POEGMA as an injectable drug formulation. POEGMA with exendin demonstrates a sustained clearance from the bloodstream while maintaining a lack of immunogenicity, unlike PEG.[278, 279]
3.2.2. Mucoadhesive polymer nanocontainer creating strategy
In addition to challenges such as early clearance from the body and enzymatic degradation, the mucosal barrier can also impede the passage of drugs through biological barriers. Mucoadhesive compounds can enhance the contact of particles with the biosurface, thereby increasing the bioavailability and permeability of drug.[280] Mucoadhesive polymers have numerous hydrophilic groups, such as hydroxyl, carboxyl, amide, and sulfate groups, which are adsorbed to the mucosa through such interactions as hydrogen bonding, electrostatic forces, or binding via specific receptor sites. The adhesion process is considered as two successive stages: (1) the mucus wets the mucoadhesive particle, and (2) the particle adheres to the mucosa through various physicochemical interactions.[281] Several natural polymers exhibit mucoadhesive properties, including polysaccharides (such as chitosan and alginate) and proteins (such as gelatin and albumin).[282] The gastrointestinal mucosa comprises mucin proteins, which include glycan structures, cysteine residues, negatively charged sialic acid groups, and sulfate groups. This composition results in multiple chemical and nonspecific interactions between mucin chains, forming a mesh-like and gel-like morphology that protects the epithelial cell layer beneath the mucosa.[283] Mucoadhesive drug delivery systems can overcome this protective barrier by adsorbing to and remaining on the mucosal surface for longer periods, thereby enhancing the bioavailability of therapeutic agents. Several theories explain the mucoadhesive properties of materials, including electrostatic, wetting, general adsorption, and diffusion, which help in developing or identifying materials with mucoadhesive capabilities. Materials such as chitosan, sodium alginate, cellulose, zein, and hyaluronic acid are effective in modifying drug delivery systems for DM therapy.[284, 285]
One of the most widely used natural polymers with wide biomedical functionality, including mucoadhesive properties is chitosan.[286-289] Its structure contains free amino groups that facilitate nonspecific binding to the mucosal surface. Importantly, numerous water-soluble modifications were developed through introducing of hydrophilic functional groups.[290] It was demonstrated that dicyandiamide-modified chitosan NPs with cell-penetrating octaarginine and hyaluronic acid facilitate insulin delivery via the paracellular route, thereby enhancing the efficiency of sequential transport from apical to basolateral regions and consequently increasing penetration efficacy.[291] In a study by Alalaiwe et al.,[292] it was demonstrated that the bioavailability of chitosan-coated gold NPs was significantly increased upon oral administration compared to intravenous injection of unmodified particles. The bioavailability of the particles increased 25-fold when chitosan was used instead of PEG. Additionally, chitosan exhibits pH sensitivity due to the protonation of amino groups only in acidic solutions, which is particularly advantageous for oral administration as it allows for controlled release of the drug upon reaching the target site.[293] The use of chitosan to enhance the bioavailability of oral insulin has been documented in the literature.[106, 294] In another study, NPs based on poly(lactic-co-glycolic) acid were modified with both PEG and chitosan.[294] Ex vivo and in silico studies showed that chitosan coating improved particle mucoadhesion, while in vitro analysis demonstrated successful protection of insulin from degradation under gastrointestinal-like conditions. Chitosan has also proven effective for modifying particles for the oral delivery of other antidiabetic drugs, such as metformin hydrochloride [295] and hesperidin.[296] In the study by Rebitski et al., a bionanocomposite system was proposed for the oral treatment of T2DM.[297] This system is based on intercalated compounds of metformin and clay incorporated into a pectin polymer matrix to ensure stability in the gastrointestinal tract, with chitosan added to impart mucoadhesive properties. In vitro experiments simulating gastrointestinal conditions demonstrated a slow release of metformin with the double coating across the entire pH range examined (1.2, 6.8 and 7.4) (Fig. 12).
To modify chitosan, which shows stability only within a limited pH range and is insoluble in water at neutral pH, sodium alginate is widely used due to its more hydrophilic nature and mucoadhesive properties.[298, 299] Moreover, sodium alginate is used as a standalone surface modifier for nanocarriers.[300] For DM therapy, Baig et al.[301] developed NPs with vildagliptin, a drug that regulates insulin-glucagon secretion from the pancreas, encapsulated within DNA nanocubes and coated with sodium alginate. Increasing the percentage of sodium alginate in the formulation increased encapsulation efficiency, and the resulting formulation was more effective at maintaining blood glucose levels for up to 24 hours due to the slower release of vildagliptin.
In addition to the mucoadhesive agents used, other polymers are also explored in the context of DM therapy. For example, zein-based particles were modified with PEG to enhance their diffusion through mucus.[302, 303] Another promising approach involves the use of hyaluronic acid. The effectiveness of such systems has been demonstrated for oral formulations of insulin and metformin.[118, 304]
The use of supramolecular systems is therefore a promising direction in medicine, including the DM therapy and its complications. Conventional treatments for DM used for many years have significant drawbacks such as low bioavailability, high toxicity and side effects, invasive delivery methods and, as a result, difficulties in compliance. Nanoscale drug delivery systems bypass these drawbacks by providing targeted drug delivery, thereby reducing side effects, improving solubility and stability of poorly soluble drugs, and prolonging their action. Among the various nanocarriers, lipid- and polymer-based systems remain the undisputed leaders, both in the market of approved nanoscale drug formulations and at the laboratory research level, due to their low toxicity, biocompatibility, and potential for modification for specific tasks. Furthermore, nanocarriers can be designed to be responsive to glucose or pH levels, carry multiple pharmaceutical substances, and target multiple action sites. It is worth noting that a significant part of research focuses on delivering natural plant compounds rather than toxic synthetic hypoglycemic drugs. Noninvasive drug delivery routes, such as oral, intranasal, and transdermal, combined with the use of nanocarriers, have great potential in DM therapy. However, despite the promising positive results, there are still many challenges that researchers need to overcome in the application of nanocarriers for DM treatment. These challenges include immune responses, production complexity, scalability of NP, high quality control standards, and the difficulty of correlating in vitro and in vivo experimental results with real conditions. Overall, nanoscale delivery systems and noninvasive drug administration routes represent promising directions in DM treatment, offering significant advantages over traditional methods. However, their widespread implementation requires further research and overcoming existing technical and regulatory barriers.
3.3. Materials and devices for diagnostics, visualization and monitoring of diabetes mellitus
An important task of nanomedicine is the development of devices for diagnosis, prediction, screening, visualization and monitoring of serious chronic diseases. Early detection of DM is of great importance, therefore brief discussion of the issue is given in this review. Currently, new prospects for timely diagnosis and adequate treatment of diabetes are opened by emerging the theranostics, which addresses both detection of diabetes biomarkers and therapy of the disease.[305] Much attention is therefore being paid to the development of new biomarkers that will allow the identification of prediabetic patients and their personalized management.
Traditionally, two glycemic biomarkers, i.e., plasma glucose concentration (fasting plasma glucose or oral glucose tolerance test) and HbA1c are clinically used, with the former being recognized as a gold standard, while the latter corresponding to the three-months averaged indicator and correlating properly with DM chronic complications. Both of them have advantages and limitations. Values obtained through plasma glucose monitoring are influenced by a variety of factors (diet, physical activity, sex), thereby show large fluctuation, need fasting, and should be done in a timely manner. In its turn, HbA1c test is time-consuming and takes special instruments. To avoid these limitations, nanotechnological approaches have been used to develop biosensors for noninvasive detection and continuous monitoring of diabetes biomarkers. These nanomaterials sensitive to indicator molecules are usually classified as organic and inorganic NPs. The category of organic NPs includes biological and synthetic materials, both low molecular and polymeric. Inorganic nanoparticles are grouped into metallic and ceramic, with the quantum dots and carbon-based nanocomposites receiving special attention.[305-307] Quantum dots are one of the key components in nanomedicine tools, which have many applications in noninvasive monitoring and treatment of diseases. Importantly, they are successfully used for imaging due to their beneficial characteristics, including colloidal and photostability, size-dependent luminescence, the ability to use the same irradiation source to excite quantum dots of different sizes. These give them advantages over luminescence devices based on organic dyes. A separate line of research activity focuses on the development of analytical devices for the detection of antidiabetic drugs in biological fluids, which is necessary to prevent their accumulation and side effects. Gazizadeh et al. constructed [308] a dual-emission fluorescent sensor by combining two fluorescent platforms, nitrogen dopped graphene quantum dots and Tb(III)-based NP (Fig. 13). It was shown that the emission intensity of both sources increased upon interaction with the antidiabetic drug metformin depending on its concentration in human serum samples. The developed method has a low detection limit of 0.76 nM and can be used for selective and accurate control of the drug content.
In this regard, wearable diabetic healthcare devices should be emphasized that analyse various biofluids (saliva, tears, interstitial fluids, sweat), which are a very attractive alternative to traditional glucometers.[309-311] Among noninvasive platforms, patches sensitive to glucose in sweat, microneedles monitoring glucose level in interstitial fluids, and smart microscale lenses detecting glucose in saliva are of particular interest. These devicses are generally classified according to physical methods used into electrochemical and optical constructions.[305] Electrochemical techniques involve two strategies based on enzymatic or non-enzymatic glucose detection. Optical sensors are based on fluorescence, colorimetry, surface plasmon resonance techniques and some other. An example is the development of a sweat glucose monitoring platform based on a fluorescent microfluidic chip with a dual-sensor membrane. The device includes simultaneous measurement of O2 and H2O2 levels, which are involved in the enzymatic oxidation of glucose, and is connected to a smartphone. When excited by 395 nm light, red fluorescence is used to detect O2 level, while the ratio of green and blue fluorescence is used to detect H2O2 . The dual sensitivity principle ensures high analysis accuracy and a low detection threshold.
Apart from widely used glucose sensing smart materials (for example, the fluorescent microarrays described above), DM may be successfully diagnosed through monitoring the concentration of violate compounds in human exhaled breath. A variety of organic low molecular weight derivatives including alcohols, aldehydes, ketones, and other are identified as biomarkers for various diseases. In particular, an abnormal acetone concentration more than twice that of healthy patients indicates diabetes symptoms.[312] New opportunities are provided by multisensory technologies, which enable the precise detection of several analytes or parameters in a tested sample, and fundamentally improve the size and timeline characteristics, as well as the prospects for scaling the device manufacturing process.[313]
To summarize this brief literature assay of the nanomedicine tools for the prevention, diagnosis, and treatment of DM and its complications, it should be emphasized that despite the fast progress in this field, many challenging problems remain unsolved and require further investigation. A variety of theranostic platforms have demonstrated their high efficacy due to variable characteristics that allow fine tuning towards personal needs. An important task is to establish correlation between physicochemical parameters (size, surface, charge, spectral characteristics), solution behavior (stability and prolong circulation in bioenvironment), and functionality (sensing of biomarkers, ability to switchable behavior, etc.) of nanomaterials. This can be achieved by developing interdisciplinary research to highlight the factors behind this interrelation and will allow the creation of nanodevices with specified and customizable characteristics.
4. Nanomaterials to treat complications of diabetes mellitus
The particular danger of DM is associated with the development of various complications in the background of the disease. Despite the fact that all complications have a common source — long-term hyperglycemia, they can affect different organs and proceed individually in different patients. Therefore, before moving on to a discussion of chemical and nanotechnological aspects, it is necessary to briefly consider the types of complications associated with DM.
The long-term hyperglycemia results in macro- and microvascular complications. Macrovascular complications affect the cardiovascular system, causing stroke, myocardial infarction, cardiac angina, coronary artery disease, and heart failure. Microvascular complications affect various tissues and organs, e.g., eyes, kidneys, nerves, liver, feet; they are classified as retinopathy, nephropathy, neuropathy, etc., and are a cause of increased morbidity and mortality of DM patients.[314, 315, 8-11]
Recently, new generations of glucose-lowering drugs have been developed, such as DPP-4; SGLT2 inhibitors, GLP-1 receptor agonists, which has allowed one to reach a new level for the treatment of T2DM and cardiovascular complications, signifying a transition from simple glucose control to supporting the cardiovascular system.[20] For optimal therapy, it is recommended that these drugs be introduced in combination with traditional antiglycemic medications, such as metformin.
The microvascular diabetic complication, retinopathy, or retinal vascular disease, is associated with progressive degeneration of photoreceptor cells, that is accompanied by unusually high angiogenesis. Diabetic retinopathy is the leading cause of blindness in elderly diabetic patients. It can generally be categorized into proliferative and non-proliferative retinopathy. Based on the fact that vascular endothelial growth factor (VEGF) is a key contributor promoting neovascularization, antibodies to VEGF, such as bevacizumab or pegaptanib are typically used to treat non-proliferative diabetic retinopathy,[314] but long term systemic effects are not achieved.
Nephropathy is another complication, in which hyperglycemia is a main pathogenic factor. Excessive formation of reactive oxygen and nitrogen radicals shifts the oxidation/reduction balance, thereby resulting in oxidative stress. This in turn can lead to renal vascular sclerosis, increased vascular permeability, and disbalanced structural and functional behavior. This problem is addressed in work,[316] reporting on melanin NPs decorated with low molecular weight chitosan for targeted delivery of dagliflozin to the kidneys. The particles had high colloidal stability, pH-responsive release of the drug, and high free radical scavenging properties. In vivo experiments on the STZ-induced diabetic mice demonstrated a significant therapeutic effect.
Chronic hyperglycemia, typical for DM, is a reason for the development of different hepatic diseases. Due to the crucial role of the liver in glucose metabolism, insulin sensitivity and lipid regulation, much attention is being paid to the hepatic complications associated with DM, including an increased risk of non-alcoholic fatty liver disease. This can be exemplified by comprehensive review focusing on pathogenesis, risk factors and therapeutic strategies in the field of hepatic complications.[10]
It should be emphasized that one of the key mechanisms contributing to DM and related complications is nonenzymatic glycation, known as the Maillard reaction, which occurs through a cascade of biochemical transformations with no contribution of glycosyltransferase.[317-319] Initially, condensation reaction of free amino groups of proteins, lipids, and nucleic acids with carbonyl groups of reducing sugars (glucose, fructose, galactose) occurs resulting in the labile Schiff bases products. Their further rearrangement yields more stable Amadori compounds, while subsequent degradation of these early glycation products results in the formation of advanced glycation end-products (AGEs) (Fig. 14).
AGEs play a crucial role in the etiology of DM and its complications by accumulating in tissues, changing the structure and functionality of proteins, thereby triggering pathological processes. The higher the glycemia, the more AGEs are generated, which remain in tissues even when normal level of glycemia is adjusted. A number of glycated products are used as diabetes biomarkers, which can be illustrated by the example of HbA1c, a widely accepted DM biomarker.
Many researchers are focusing on studying the detailed mechanisms of AGE effects on tissue behavior. There are two key pathological contributions responsible for the development of diabetes and its complications, i.e., receptor-free and receptor mediated ways. The first is due to chemical modification of proteins, resulting in alteration of their biochemical behavior, interactions with other biopolymers, and, ultimately, altered tissue properties. Noteworthy, that almost all proteins: collagen, albumin, hemoglobin, lipoproteins, and eye lens proteins are damaged by glycation. This can be briefly exemplified by collagen, the key component in the human body. It is known that up to 50% of all collagen is contained in bone tissue, while the rest occurs in connective tissue, skin, vascular walls, etc. There are 28 types of collagen, which differ in amino acid sequence and degree of functionalization, and different types of collagen are found in different tissues. The most common of these is collagen type 1. Glycation of collagen causes a change in its physicochemical properties, flexible and mechanical characteristics, which are manifested in lower solubility, greater resistance to collagenase, eventually resulting in aging and diabetes.[320, 321]
The second pathway is mainly through the interaction of AGE with the receptor for advance glycation end products (RAGE), which triggers different signalling pathways. RAGE is a transmembrane protein that is expressed in a wide variety of cells, such as macrophages, endothelial cells, neurons, etc. Consequently, different signalling pathways can be involved, including nicotineamide-adenine dinucleotide phosphate oxidase, nuclear factor-kB, phosphoinositide 3-kinase, Janus kinase/signal transducer and activator of transcription, and other signalling pathways, contributing to the development and progression of DM-related complications. The AGE/RAGE axis is therefore recognized as a pathophysiologic factor in diabetes complications.
More detailed discussion of the diabetes complications in terms of nanomedicine platforms and approaches is exemplified by diabetic wound healing.
4.1. Current strategies and nanomaterials used for diabetic wound healing
Delayed wound healing is one of the most serious DM complications that can occur in persons with long-term hyperglycemia. The pathophysiology of diabetic wound healing is a complex process contributed by a combination of risk factors and abnormalities, including neuropathy, vascular diseases, and bacterium infections. The treatment of diabetic wounds is therefore a global challenge for modern medicine and requires the development of coordinated solutions with the participation of experts from the fields of chemistry, biology and nanomedicine. For this, it is necessary to take into account the specific nature of the process of wound healing, as well as the factors that determine the transition of the disease to a chronic form. The therapy of diabetic wounds is a striking example of interdisciplinary research using supramolecular strategies and chemical materials, where knowledge of medical aspects is crucial.
To fabricate materials for the effective treatment of different kinds of injuries (burn, cut, ulcer, wound, etc.) microenvironmental details and categories of the regeneration process should be defined, taken into account and synchronized upon the healing.[322, 323] Thus, in work,[322] experimental rat models are analyzed and compared with other animal models with a view to their appropriate use in the study of chronic wounds of various etiology and the most accurate translation of the findings into clinical practice. Depending on the period of time needed for the healing, acute and chronic character of the process are differentiated. For acute healing, four stages are categorized, overlapping with each other, including hemostasis, inflammation, proliferation and remodelling (Fig. 15).[324-328] These processes are highly coordinated with different mediators (cytokines, growth factor, genes) and involve a variety of cells, including keratinocytes, fibroblasts, immune system cells, endothelial cells, mesenchymal stromal cells (MSC) and others.
The hemostasis stage (coagulation) includes the vascular contraction, formation of fibrin clots and platelet aggregation to prevent loss blood and provide a barrier against bacteria. After that, the inflammatory response phase is observed, with such symptoms as elevated temperature, reddening, edema, and pain. At this stage, neutrophils and macrophages are defending the wound site against pathogens, and necrotic cells with damaged tissues and cellular debris are being cleared out. Further, the closer of the wound and growth of new skin begins, mediated by extracellular matrix deposition, contraction of wound borders, neovascularization, and re-epithelization. At the final stage, the processes of maturation and remodelling occur, when the collagen type 3 is reorganised into the collagen type 1, granulated tissues transform into scar tissue, accompanied by apoptosis of unneeded cells.
Unlike these four stages typical of acute wounds, in the case of chronic wounds, regardless of their etiology, there is a disruption of the normal course of the healing process.[323, 330] Risk factors responsible for this deviation from the above four-stage process are considered to be hypoxia, reactive oxygen species, inflammatory cytokines, proteases, and dense biofilm. Review [330] highlights different genes and signalling pathways involved in the wound healing process, the disbalance of which results in impaired healing. Among these, the phosphoinositide-3-kinase/protein kinase B, Wnt/β-catenin, TGF-β, VEGF, Notch, nuclear factor erythroid 2-related factor 2 (Nrf2) are crucial contributors mediating wound healing behavior. These factors behind the redirection of normal wound healing are being taken into account in the development of the strategies and therapeutic platforms for the chronic wound treatment, including those for diabetic patient.
Traditional management of diabetic wounds including debridement of wound, antibiotic and insulin therapy, as well as simple wound dressing is not enough effective due to numerous limitations and is unable to improve the quality of life of diabetic patients. A recent literature review demonstrates that a significant increase in the therapeutic efficacy can be achieved within the framework of nanomedicine approach, with different therapeutic platforms and different nanocarriers being explored. According to work,[331] the following therapeutic strategies are categorized: drug therapy, growth factor-based therapy, gene therapy, peptide therapy, stem cell therapy, gas therapy.
Drug-based therapy, including drug combination, involves different types of NPs, which can nominally be divided into three categories, namely, biological NPs (e.g., exosomes), organic NPs, both synthetic and naturally derived (polymer-, lipid-based and hybrid systems), inorganic NPs based on metals and their oxides, mesoporous NPs, nanotubes and others. It is important to mention the trend in current drug therapy to reprofile drugs, i.e., to use approved therapeutics for the treatment of a wider range of diseases.[331]
Growth factor-based therapy. Families of different growth factors play a crucial role in the wound healing process. These polypeptides control the interaction of different cells, the formation of extracellular matrix, angiogenesis, and epithelization. Much research is therefore being devoted to the development and delivery of preparations based on growth factors. This line of research is a branch of a broader strategy based on peptide therapy, which in addition to growth factors involves hormones, ion channel ligands, neurotransmitters, etc. Due to their high affinity to surface cell receptors peptide molecules activate signalling intracellular pathway thereby initiating therapeutic effect.
Gene therapy is a promising strategy directed on replacing a defective gene or its section by delivering genetic material into the cell. For this purpose, overexpression of matrix ribonucleic acid (RNA) and plasmid DNA is typically used, while small noncoding RNA, small interfering RNA and oligonucleotide are introduced as silencing agents. In this field, nanotechnologies provide numerous advantages enabling gene delivery to targeted cell.
Stem cell therapy. Stem cells, the precursors of all other cells, contribute to the formation of new, unaffected vessels in the wound area, restoring local blood flow, promoting reparative processes, and stimulating the healing of the skin defect. Various types of stem cells are reported to be explored for the treatment of diabetic wound, e.g., adipose-derived MSC, peripheral blood stem cells, human umbilical cord MSC, placental-derived MSC, embryonic stem cells, etc.
Gas therapy is associated with the use of gas-signalling molecules, such as nitric oxide, hydrogen sulphide and carbon oxide. A therapeutic strategy based on the gas-signalling molecules can be exemplified by the study [332] devoted to the control of biofilm formation. Due to antibiotics resistance, biofilms present a challenging problem in many chronic diseased subjected to infection. It has been shown that bacterial NO sensors can influence the biofilm formation; therefore, this study presents new nitric oxide sensing bacterial proteins and their contribution to the biofilm regulation in gram-negative bacteria. In this context, work [333] devoted to the design of the NO-donor drug molecule for the T2DM treatment could be mentioned. For this purpose, nitrosyl iron complex with thiosulfate ligands was prepared and studied in vitro, including effects on DM and interaction with cell membranes, wherein its antiradical activity was demonstrated.
Recent publications exploring the above strategies using nanomedicine tools are given below.
One of the most sought-after platforms for the management of diabetic wound are dressings. Initially, they were used as simple barriers covering the injuries, thereby preventing them from contact with external contaminants. With the advancement of the nanotechnology, rather strong criteria emerged towards the design of dressings, including their composition, biocompatibility, stability, antimicrobial activity, answering the change in microenvironmental conditions at different healing stages and ability to switch between them. There is a large body of literature devoted to the dressing formulations for the diabetic wound treatment, including those based on nanogels and nanofibers with different polymeric material used.[323, 324, 327, 334-338] Among these, hydrogels composed of hydrophilic polymers have received special interest and widespread application. Due to three-dimensional structure hydrogel-based dressings can effectively absorb exudate and provide retention. In a series of studies,[337-339] supramolecular hybrid hydrogels, including those with chiral properties, were developed, demonstrating excellent antimicrobial and antioxidant activity in combination with high biocompatibility.
In the [340] application of oligo- and polysaccharide-based nanomaterials in biomedical sphere are reviewed. It highlights the advanced characteristics of chitosan-based hemostatic hydrogel, including appropriate viscosity, stability in wet conditions, fast reorganization into a gel to stop bleeding, which can provide an effective tool for engineering the diabetic wound dressing. It has been shown that the hemostasis effect depends on the molecular mass of chitosan and the degree of functionalization of the macromolecule. A decrease in the degree of acylation results in an increase in the coagulation effect and formation of blood clots due to the enhanced interaction of positively charged chitosan with red blood cells. Deacetylation of the polymer is accompanied by a decrease in charge density and lower conductivity, while resulting in the formation of hydrogen bonds and an increase in viscosity.
A family of oligosaccharides, cyclodextrins, are also discussed, highlighting beneficial properties such as natural origin and low toxicity, biocompatibility and bioavailability.[340] Additional advantages of cyclodextrins are associated with their guest-host interaction involving drug molecules, which is a promising tool for tailoring the stability and reactivity of encapsulated guest. Importantly, the physicochemical properties of cyclodextrins can be modulated by their chemical or noncovalent functionalization, allowing the control of HLB and the preparation of amphiphilic macrocycles.
The polymer-based nanocontainers are discussed in section 3.2 of the review. Generally, both natural and synthetic polymers are used for the hydrogel engineering, with different benefits and limitations observed for each. Hydrogels based on the natural polymers are characterized by biocompatibility, low toxicity and biodegradability, while do not show sufficient mechanical strength. In contrast, the advantageous stability and mechanical properties of hydrogels based on synthetic polymers are offset by poor biocompatibility and biodegradability. This encourages researchers to fabricate composite hydrogels containing different domains based on synthetic or natural polymers, bound with noncovalent bonds. Such a bilayer hydrogel was designed [329] with the outer layer composed of two polymers, polyvinyl alcohol and hydroxypropyl methyl cellulose, while the inner hydrogel was formed by chitosan quaternary ammonium salt, flaxseed gum, and polyvinyl alcohol. The outer layer demonstrated good mechanical and protection properties due to the formation of hydrogen bond network. Quaternized chitosan in the inner layer provided an additional antibacterial effect, thereby increasing multifactor healing activity of the dressing. This hydrogel platform was loaded with L-arginine-modified polyoxometalate, which can generate NO in response to hydrogen peroxide conditions, which was essential in accelerating wound healing by promoting cell proliferation and migration.
Another example of polyfunctional hydrogel is given in work,[341] wherein composite material based on quaternized chitosan (QCS), graphene quantum dots (GQDs) conjugated with ε-poly-L-lysine (ε-PL), and benzaldehyde (BA)-terminated 4 arm PEG was developed. The hydrogel demonstrated excellent combination of beneficial colloidal and therapeutic behavior, including in situ sprayable ability, biocompatibility, responsibility to xenon light and environmental pH, thereby undergoing swelling/degradation transition resulting in the release of antibacterial components, self-recovering of hydrogel structure and promotion of wound healing (Fig. 16).
In study,[342] a hydrogel dressing based on a carboxymethyl chitosan is fabricated. The mechanical properties were improved by supplementing the formulation with pectin and polydopamine. The resulting composite hydrogel with beneficial multifunctional characteristics (biocompatibility, water retention, tissue adhesion, antioxidant, and antibacterial effects) was further loaded with active therapeutics, recombinant human epidermal growth factor, demonstrating sustained release. In vivo study provides evidence of high acceleration of wound healing with a 97.84% wound contraction rate at two weeks.
Nanofibers are another platform of interest from the point of view of chronic wound therapy, demonstrating such benefits as advanced mechanical and porous characteristics, high surface area-to-volume ratio, etc. Nanofibers can be fabricated through different techniques, with primarily role devoted to electrospinning. In work,[336] nanofibers potential in the wound healing process is discussed, with special focus on hyaluronic acid-based materials. Hyaluronic acid is directly or secondarily involved in different stages of the wound healing process, thereby stimulating the therapeutic efficacy.
A number of studies have focused on the lipid formulations due to their low toxicity, high biocompatibility and simplicity in the preparation. Section 3.1.1. of the review presents SLN, NLC, and NE as efficient nanocarriers for DM treatment, including their use in wound healing.
Fabrication, characterization and application of microemulsions and NE have been reviewed.[343] Microemulsions are spontaneously formed thermodynamically stable systems. The formation of NE, similar to liposomes, requires the application of energy; they are kinetically stable systems. Unlike NE and liposomes, microemulsions are not widely used as drug delivery systems, since they are less stable to the action of the biomicroenvironment and are quickly destroyed in the body. In this paper, both fundamental and biomedical aspects are emphasized, with much attention paid to reverse microemulsions, which are widely used as nanoreactors for the NP synthesis. The advantages of microemulsions are noted, including the possibility of encapsulating substances of various natures, as well as high efficiency for transdermal therapy. In work,[344] lipid nanoparticles (LNPs) based on the polymer isomannide were used for the co-delivery of messenger RNA to adipose stem cells (ASCs), which are recognized as an efficient therapeutic platform in terms of regenerative properties in combination with low immunogenicity. Optimized drug nanocomposition showed a markedly higher delivery efficacy compared to electroporation, lipofectamine-based vector or FDA approved LNPs. It was demonstrated that the developed lipid formulation is a promising ASC therapeutic product with controlled secretion of purpose proteins for accelerated wound healing.
An excellent alternative to cell therapy are strategies based on the application of extracellular vesicles, which have higher stability, lower immunogenicity, and lower risk of embolization.[345] In this study, MSC-derived small extracellular vesicles were used as drug carriers for a therapeutic circular RNA. In vivo study showed that local subcutaneous injection results in an accelerated wound healing and skin regeneration.
Hybrid lecithin-chitosan ethosomes were fabricated for the encapsulation of drug kaempferol.[346] The developed formulation answered nanomedicine criteria (size 186 nm; zeta potential 31.9 mV), demonstrated high encapsulation efficacy of 96.2% and prolonged drug release. Topical administration of the ethosome based gel loaded with kaempferol showed higher therapeutic efficacy compared to the plain gel formulation, which was supported by a pharmacokinetic study in the rat and histopathological tests. Enhanced wound closure effect is thought to be due to the moisture gel environment in combination with the antimicrobial, lipophilic and mucoadhesive properties of the components.
In work,[347] a hybrid polymer-lipid platform was engineered based on a polycaprolactone core and a lecithin/geleol outer shell, that were incorporated into the thermosensitive pluronic hydrogel. This composite nanostructure was used for the co-delivery and step-by-step release of granulocyte-macrophage colony-stimulating factor and VEGF to successively affect different stages of the healing process, namely, to activate macrophages in the inflammation phase and to further promote the proliferation process.
It was documented that one of the key components promoting the chronic wound healing is vitamin B5, pantothenic acid or its calcium salt.[348-351] Pantothenic acid is a precursor of coenzyme A (CoA), which plays a vital role in metabolism of proteins, lipids and carbohydrates. Disturbance of CoA functions may result in serious exacerbation of chronic diseases, including diabetes, inflammatory processes, oncology, etc. Therefore, therapeutic intervention in CoA metabolism is a promising approach for the treatment of various chronic diseases, including wound healing. The role of the vitamin B5/CoA axis in the pathology of a wide range of diseases has been highlighted in work.[348] In particular, the contribution of pantothenate to improving the wound healing process achieved by topical administration of dexpanthenol, provitamin B5, has been demonstrated. This alkanol derivative is a constituent of many therapeutic and cosmetic products, exhibiting a strong effect on human fibroblasts, their proliferation, cellular migration to the site of inflammation, fixation of fibroblasts in the wound and increased collagen synthesis.
As successful examples, novel wound dressings based on poly(glycerol sebacate)/gelatin supplemented with vitamin B5 and vitamin C were fabricated by electrospinning.[349] A burst release of the drugs was observed: after 1 hour (vitamin C) and 6 hours (vitamin B), with the former providing cell adhesion and cell proliferation, while the latter showed an antimicrobial effect responsible for the wound healing activity. The same electrospun technique was applied to develop a nanofibrous textile made of polyurethane, sodium bicarbonate and pantothenic acid.[350] The morphology, porosity and hemocompatibility of the nanocomposite were examined. The excellent combination of physicochemical and functional characteristics of the dressing enabled the wound healing process to be markedly accelerated.
Despite the optimistic results discussed herein, there are numerous challenges and limitations preventing from their clinical translation. One of the leading reasons is connected with the difficulties in the choice of proper animal model. The majority of wound healing assays use the murine model with STZ — or alloxan-injection explored for T1DM, while genetically obese (ob/ob) and diabetic (db/db) mice are most commonly used to model T2DM. The murine model cannot be adequately extrapolated to humans because it does not reproduce the human wound healing process. The more relevant porcine model also has limitations in terms of costs and technical difficulties. Additional efforts, including intensive fundamental studies and clinical trials are therefore needed to overcome these problems and improve therapeutic effect.
4.2. Diabetes mellitus as a risk factor for Alzheimer’s disease
To conclude the review, it seems important to analyze the relationship between DM and AD, which is widely discussed in the literature 5 and is directly related to the creation of carriers capable of crossing the blood-brain barrier for the encapsulation and delivery of antidiabetic drugs. Alzheimer’s disease affects 3 – 4% of people over the age of 60 and is a global health emergency. The disease is characterized by the excessive production and accumulation of oligomerized forms of β-amyloid (Aβ) peptide, tau protein and, in addition, by the disruption of the function of the cholinergic system, expressed by a decrease in the levels of the neurotransmitter acetylcholine with subsequent death of cholinergic neurons.[352]
Existing therapy is based on compensation of the cholinergic deficit associated with AD and can only provide a temporary symptomatic effect.[353] To date, attempts to develop new therapies have not resulted in the development of AD-modifying drugs, which may be due to a lack of understanding of therapeutic targets. In this context, it is important to note that AD is a multifactorial disease and is often burdened by concomitant comorbid (multimorbid) diseases. These comorbid diseases can occur before or simultaneously with AD, worsen the overall clinical status and contribute to the progression of the disease.[354] In this regard, targeting modifiable risk factors associated with comorbid diseases may be important in delaying the onset or progression of AD.
Numerous epidemiological and clinical studies have shown that patients with DM and/or obesity are at increased risk of developing AD.[355, 356] It should be noted that not all people with DM develop dementia, and not all patients with dementia also have any form of DM. Thus, DM and AD are two independent diseases. However, it can be assumed that influencing the common pathogenesis factors in DM can have an effect on delaying the development of AD.
It has been shown that DM patients as well as AD patients can have impaired cerebral glucose metabolism.[357, 358] The use of positron emission tomography (PET) with [18F]2-fluoro-2-deoxy-D-glucose to assess changes in D-glucose uptake and metabolism allows the identification of brain regions with decreased D-glucose uptake.[359-361] PET identified decreased uptake of D-glucose has been observed in the frontal, temporal, parietal, occipital, entorhinal cortex, and in hippocampus.[362] These regions overlap with the brain regions, where the greatest histological changes in response to AD have been observed. The degree of PET signal reduction during AD correlates with severity and rate of progression of cognitive defects.[363]
There are several hypotheses on the origin and the role of impaired glucose metabolism in AD. The loss of glucose transporters (GLUT) is one possible cause of impaired cerebral glucose metabolism. It has been shown that people, who have developed AD exhibit altered expression of GLUT1 and GLUT3, especially in the cerebral cortex.[364] However, there are other explanations for decreased cerebral glucose uptake. It has been shown that brain insulin resistance and insulin dysregulation could contribute to the neurodegeneration observed in AD.[365] It is known that impaired peripheral insulin signalling may account for brain insulin resistance in AD.[366] Together, these insulin signalling impairments translate in a collapse of glucose homeostasis leading to cerebral hypometabolism, which is responsible for the accumulation of Aβ and hyperphosphorylated tau.[365] Thus, insulin resistance can contribute to the progression of AD and could be considered as a risk factor for the development of AD. Antidiabetic drugs such as insulin or agonists of glucose transporters have been suggested as potential therapeutics that could also slow down the development of AD in the early stages.[367]
In addition to impaired glucose metabolism, neuroinflammation that often accompanies DM is also a significant risk factor for AD. Data accumulated over the past decades indicate a close relationship between the development of AD pathogenesis and neuroinflammation.[368] It has been shown that AD patients have increased levels of inflammatory markers, such as cytokines, chemokines, and acute phase proteins, in the brain and cerebrospinal fluid.[369] A bidirectional relationship between inflammation and AD has been shown; neuroinflammation can lead to Aβ accumulation, and Aβ accumulation can further increase neuroinflammation.[369-371] Neuroinflammation is currently considered to be the main mechanism linking AD and DM.[368] Chronic inflammation during DM can lead to disruption of the blood-brain barrier integrity, which increases the risk of developing AD.[372-374] Based on the analysis of risk factors and signalling pathways, intranasal insulin administration has been documented as a promising nanomedicine approach.[375]
5. Conclusion
DM is currently in the focus of both multidisciplinary fundamental researches and clinical trials due to the tremendous burdens faced by diabetes patients, their families and health care systems as a whole. Therefore, the review addresses this challenging problem with a focus on nanomedicine aspects. Along with general consideration of the pathogenesis, diagnosis and monitoring of the DM, the innovation strategies used for the management of DM and the construction of drug delivery systems are reviewed. Nanotechnologies are successfully involved in drug therapy, giving a new chance to traditional preparations instead of long-term process of discovery and implementation of new therapeutic molecules. The improvement of the efficacy of encapsulated drugs is achieved by increasing their solubility, biocompatibility, bioavailability, control of the dosage and release profile, and targeting delivery, which makes it possible to decrease side effects, avoid premature drug release and prolong their circulation in the bloodstream. A major advantage of formulated drugs vs free drugs is also the possibility of combination delivery, allowing the production of multitargeted cocktails, hydrophilic/hydrophobic drug pairs or drug/diagnostic probe combinations. At the same time, many problems and challenges yet remaining in the field of nanomedicine, partly are due to the strong requirements placed on drug delivery systems, including nanoscale size, low toxicity, high encapsulation efficacy, safety, and patient-friendly properties. Therefore, the development of new generations of nanocarriers is an ongoing process. In this context, supramolecular tools provide excellent perspectives not only for designing new formulations, but also for modifying them to meet new nanotechnological criteria, to adapt them to alternative administration routes and diseases, or to optimize their compositions for the delivery of new drugs and their combination.
In this review, much attention is paid to lipid and polymeric nanocarriers, as well as hybrid NPs. Different families of vesicular systems composed of natural or synthetic amphiphilic building blocks are considered, including liposomes, niosomes, transfersomes, bilosomes, ethosomes, etc. Their beneficial features include the ability to overcome biological barriers (blood–brain barrier, skin, intestinal barrier, nasal), which allows them to be adjusted to different administration routes, including patient-friendly transdermal and intranasal ways. The use of lipid formulations, i.e., liposomes, SLN, NE is of great importance from the viewpoint of biocompatibility, low toxicity, high loading efficacy, universal suitability for hydrophilic and hydrophobic drugs. Application of polymers markedly widen these bonuses due to the fabrication of stealth systems that avoid detection by immune cells or impart a mucoadhesive effect based on an affinity for mucus membranes.
Many challenging problems are associated with DM complications, which ultimately have common background in terms of chronic hyperglycemia. To give the representative information on pathogenesis, risk factors and nanomedicine tools for the family of macro- and microvascular complications of DM, diabetes wound healing strategies were discussed in more details. The final part of the review is devoted to insulin resistance as a risk factor for AD, making it reasonable to consider insulin brain pathology as T3DM.
In order to specify nanomedicine strategies for the management of diabetes, it is necessary to emphasize the inherent features of DM, that determine special criteria for the design of drug delivery systems. T2DM is mainly a disease of elderly people, therefore the management of DM occurs on the background of other diseases. This requires an individual approach in the choice of drugs, administration routes, nanocarriers, etc. Many diabetes patients are faced with the need for systematic insulin injections. In this case, the development of a noninvasive patient-friendly therapy can be considered as a promising alternative to traditional administration ways. Besides, DM is a multifactor disease with a complicated pathological pattern, which affects the management of DM patients. Even more strong criteria should be applied in the case of DM complications. This can be exemplified by diabetic wound healing, which consists of several stages with different microenvironmental conditions. In this case, specific criteria should be elaborated for drug formulations that allow switchable self-adaptive behavior answering these conditions.[376] A challenging problem is the early diagnosis, prediction and prevention of DM, which requires further efforts to study the molecular and genetic mechanisms of etiology, pathogenesis and exacerbation of the disease. Based on these considerations, the following line of fundamental research activity in DM management should be marked out: (1) drug delivery intervention using new generations of therapeutic molecules with new underlying mechanisms; (2) involvement of advanced supramolecular strategies to design smart NPs responsive to various endogenous or exogenous stimuli (pH, temperature, glucose, light, magnetic field); (3) development of new biomarkers and engineering of multitargeted delivery systems for combinatorial therapy; (4) design of composite formulations with tunable behavior, suitable for their reprofiling for different drug/diseases/administration routes; (5) creation of theranostic platforms answering both early diagnosis/monitoring and treatment of DM; (6) fabrication of noninvasive analytical devices through multisensor technologies with advanced size and timeline characteristics; (7) construction of the depot-like nanocontainers with prolonged circulation in the bloodstream; (8) priority development of personalized approaches based on individual patient history to address the unmet needs of patients. To complete the picture, it should be emphasized that, while the results are encouraging, especially on the account of nanomedicine platform, the clinical achievements are rather modest. This is largely due to difficulties in extrapolation of in vivo results to humans. Therefore, more relevant animal models and joint interdisciplinary efforts of specialists in chemistry, biology and medicine are needed for their successful translation into clinical practice.
This research was funded by the Russian Science Foundation (project No. 24-13-00301), https://rscf.ru/project/24-13-00301/.
6. List of abbreviations
AD — Alzheimer’s disease,
AGE — advanced glycation end-product,
ASC — adipose stem cells,
Aβ — β-amyloid,
Сmax — maximum concentration of a substance in blood plasma,
CoA — coenzyme A,
Con A — concanavalin A,
DM — diabetes mellitus,
DNA — deoxyribonucleic acid,
DPP-4 — dipeptidyl-peptidase-4,
FA — folic acid,
FA-RM-ELNC — reversible micelle-lipid nanocapsules with folic acid,
FDA — Food and Drug Administration,
GLP-1 — glucagon-like peptide-1,
GLUT — glucose transporter,
GOx — glucose oxidase,
HbA1c — glycated hemoglobin,
HLB — hydrophile-lipophile balance,
IDF — International Diabetes Federation,
LNP — lipid nanoparticles,
MSC — mesenchymal stromal cells,
MOF — metal-organic framework,
NE — nanoemulsion,
NLC — nanostructured lipid carrier,
NP — nanoparticle,
NPH — neutral protamine Hagedorn,
PBA — phenylboronic acid,
PBA-2 — Wulff-type phenylboronic acid,
PdI — polydispersity index,
PEG — polyethylene glycol,
PET — positron emission tomography,
POx — poly(2-oxazoline),
POEGMA — poly(oligo(ethylene glycol)methyl ether methacrylate),
PVP — polyvinylpyrrolidone,
RAGE — receptor for advanced glycation endproducts,
RNA — ribonucleic acid,
SGLT2 — sodium-glucose cotransporter-2,
SLN — solid lipid nanoparticles,
SNEDDS — self-nanoemulsifying drug delivery systems,
STZ — streptozocin,
T1DM — type 1 diabetes mellitus,
T2DM — type 2 diabetes mellitus,
T3DM — type 3 diabetes mellitus,
TGF-β — transforming growth factor beta,
VEGF — vascular endothelial growth factor.
References
















































































![Glucose-Responsive Supramolecular Vesicles Based on Water-Soluble Pillar[5]arene and Pyridylboronic Acid Derivatives for Controlled Insulin Delivery](/storage/images/resized/bRyGpdm98BkAUYiK1YFNpl5Z7hPu6Gd87gbIeuG3_small_thumb.webp)























































































































































































































































![Examples of nanocarriers used for the DM treatment [105-114]](/storage/images/resized/VLn64f7OucRmrWWhP4XLEGavXZQGv3S7zJJfxolA_xl.webp)
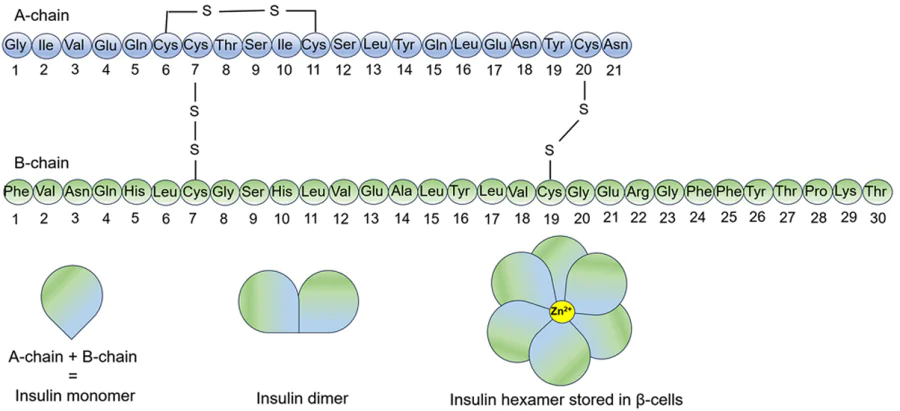
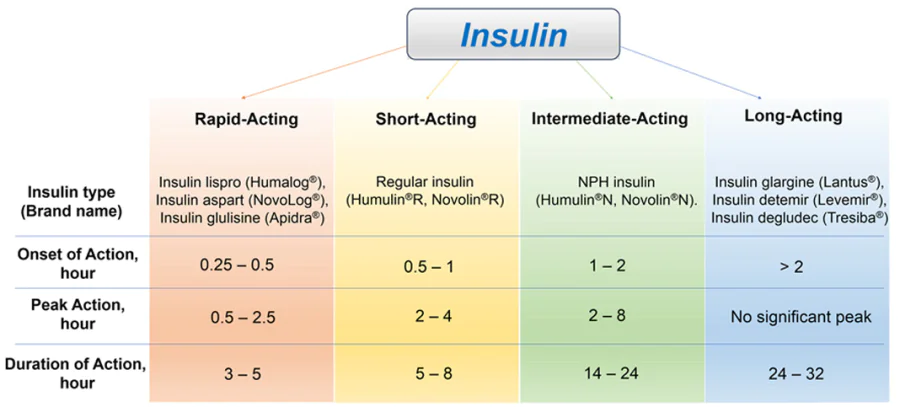
![Scheme depicting fabrication of insulin-loaded arginine-coated self-emulsifying nanoglobules system (INS-LANano): medium chain triglyceride (MCT), medium chain monoglyceride (MCM), lauroyl ethyl arginate (LAE), phosphate buffered saline (PBS).[52] This figure is published under a Creative Commons Attribution license](/storage/images/resized/whRAeQjAKs9q7D6Cn3WozA352PKvxZh8VgZFKC4z_xl.webp)
![A schematic illustration of the different strategies for the delivery of insulin via the transdermal route.[54] This figure is published under a Creative Commons Attribution license](/storage/images/resized/IDLDoorJ2Yq3TOA8dfFGNgNccPgZ7iANCxEdYiXp_xl.webp)
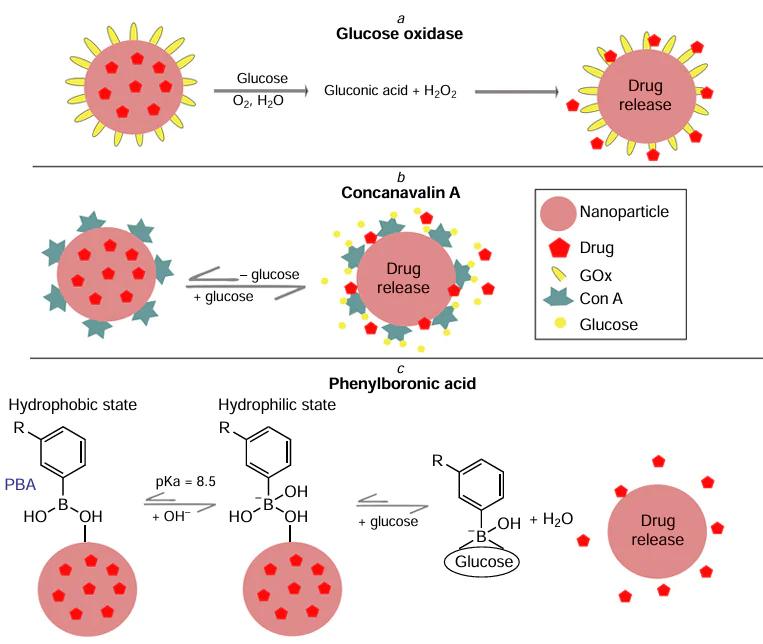
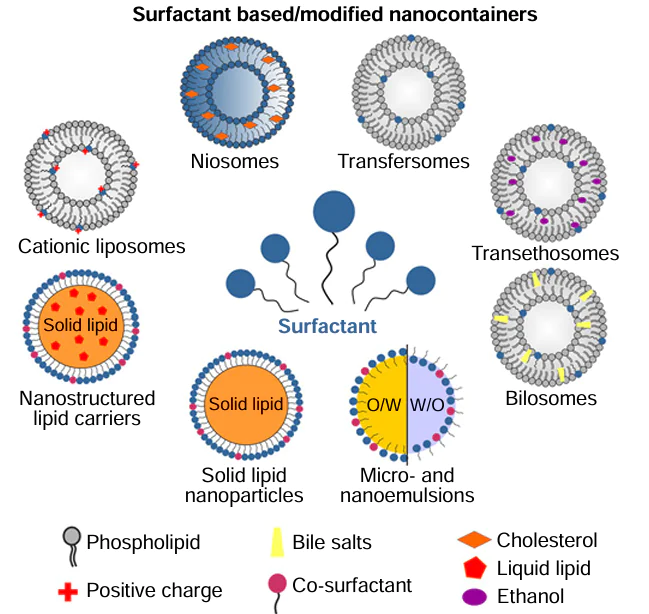
![3-D response surface plots of selected responses: (A) particle size, (B) encapsulation efficiency, (C) and PdI.[201] This figure is published under a Creative Commons Attribution NC-ND license](/storage/images/resized/p6vuqyT0auTH2j6WXkQRNoafzu1NHBhuIlhJRpKY_xl.webp)
![(a) Appearance of the SNEDDS preconcentrate (in glass tubes) and SNEDDS after dilution with water (in glass beaker) that were developed with black seed oil and soybean oil for the model drugs, sitagliptin (SN) and dapagliflozin (DN), as combined dosage form. (b) The combined F1-SNEDDS dosage form filled in a hard gelatin capsule and the appearance of the diluted SNEDDS (10 mg anhydrous formulation was diluted in 10 mL water) and (c) formation of nanodroplets/micelles of F1-SNEDDS in the presence of bile salt (BS): phospholipid (PL) and pancreatic lipase during lipid digestion in the small intestine.[225] This figure is published under a Creative Commons Attribution license](/storage/images/resized/v4AI4V3QPxkuf7SYvgpgwJXmJBGca9FPvWTf39jD_xl.webp)
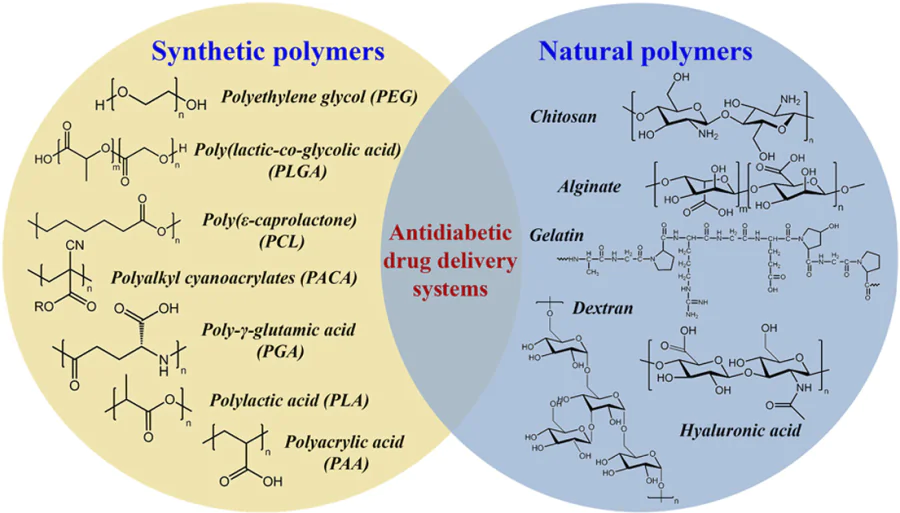
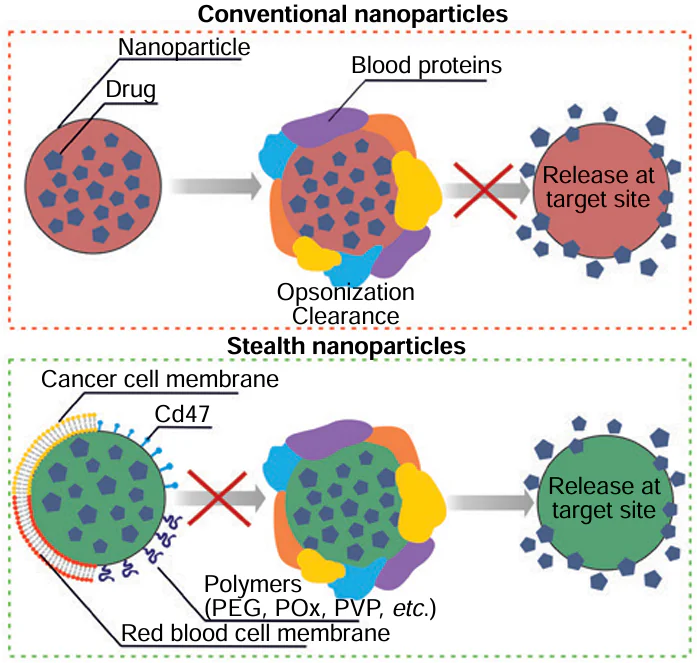
![Schematic models of the metformin-clay hybrid (Mt-MF) and the chitosan (CHT)/pectin (PEC) bionanocomposite beads (on the left) and SEM images of cross-sections (on the right) of the PEC@CHT/Mt-MFw (a) and PEC@CHT@PEC/Mt-MFw (b) bionanocomposite beads.[297] This figure is published under a Creative Commons Attribution license](/storage/images/resized/LhHnaSdGZk7wNTi0NiY9iJtkZRXHO2qUViEvvuVg_xl.webp)
![Design of a device for the determination of metformin based on its enhancing effect on the fluorescence emission of nitrogen-doped graphene quantum dots N-GQDs and Tb(III) (Tb – Phen).[308] This figure is published under a Creative Commons Attribution license](/storage/images/resized/iqLsILwGpZqZvi8dTteVuHBAS6ltC65U9IrZiIeL_xl.webp)
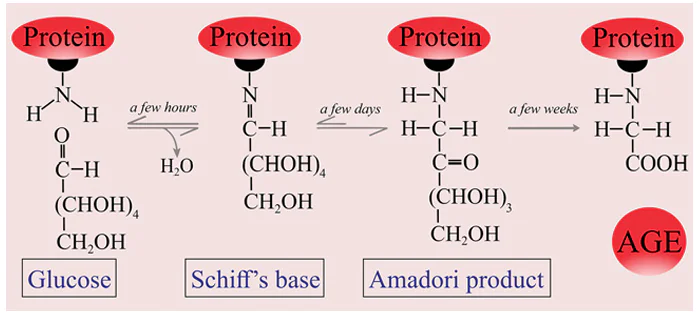
![(a) An overview of the wound healing process and the signalling processes involved in the inflammatory, proliferative, and remodelling phases. (b) Nanocarriers used for diabetic wound treatment; (c) Images[329] of wounds healing process](/storage/images/resized/MfwsTvQOis4pguR3RvhGDQgI2nPuCaYpUrQKuvlj_xl.webp)
![Schematic diagram of the GQDs-ε-PL/QCS/4 arm PEG-BA hydrogel and the hemostasis, the chemo-photothermal synergistic anti-infection and self-healing functions of the hydrogel for accelerating the healing of the infected diabetic wounds.[341] This figure is published under a Creative Commons Attribution NC-ND license](/storage/images/resized/uv7oebWEEyR3KpQGK3En2vgYeDTuIFAxtGq0KAyU_xl.webp)